Covid-19: Measures in existing buildings
Ventilation Industry Changed Radically by Covid-19 Pandemic
The ventilation industry promptly made sensible recommendations for action
The following factors increase the risk of transmission: increasing number of people and length of stay, short distances between people, insufficient outdoor air supply, special indoor climatic conditions such as cold and dryness, and activities that increase the release of fine and larger droplets such as talking, singing, shouting and increased breathing during physical work. So far, after analysing countless super-spreader events, epidemiologists and ventilation engineers are in agreement. Link 1 (see end of article) provides information on over 1,100 super-spreader events worldwide. Recommendations on the operation of ventilation systems during the Covid-19 pandemic have been issued by the trade associations of the ventilation industry in Germany, BTGA [Federal Industrial Association for Technical Building Equipment e. V.], FGK [Trade Association for Building Air Conditioning] and RLT-Herstellerverband [AHU Manufacturers Association] (Link 2) as well as the ASHRAE Epidemic Task Force (Link 3). The recommendations are based on existing buildings and the ventilation technology installed in them and allow for their optimised operation. They do not make a sufficiently clear distinction from all secondary air units which do not cause air exchange. These include air-conditioning systems (fan-convectors, split and multi-split units, mobile air-conditioning units), all of which are operated without an outdoor air component and with insufficient filters or no filters at all. Air purification units can also be secondary air units with no outside air component. They can remove pollutants, including microbes, from the indoor air using various technologies. Many users are unaware that all secondary air units have no air exchange whatsoever. This is because they intuitively associate the noticeable air flow with the concept of ventilation.
Droplets and aerosols — the discussion continues
Micro-droplets with a diameter of less than five micrometres are called aerosols. The transmission of diseases across longer distances by infectious, airborne droplets is called aerosol transmission. Health authorities, aerosol researchers, clinicians and epidemiologists continue to argue about whether the transmission of viral respiratory infections is primarily via larger droplets (range of up to about 2 m) or via aerosols and long distances. More clearly than other health authorities, RKI [Robert Koch Institute] stated in its last Covid-19 fact sheet (dated 10/07/2020) that aerosol transmission over longer distances is likely in poorly ventilated rooms (link 4). The ventilation industry recognised early on that it could make an important contribution to preventing infection.
Analyses of numerous super-spreader events have shown that the relationship between droplet and aerosol transmission depends on the droplet generation mechanism (quiet breathing, singing, speaking, shouting, coughing) and thus on the size distribution of the droplets generated. The distances the droplets and aerosols can travel depends on their diameter and therefore mass. Larger droplets fall to the ground within the two-metre distancing rule in accordance with the ballistic trajectory, whereas micro-droplets can float, which means they can be transported over greater distances, depending on the air currents. Induced convection (ventilation), buoyancy from heat sources and indoor climate have an influence on the distribution in the room, the residence time and the infection duration of airborne droplets. It has been proven that small droplets contain more infectious viruses than large droplets. In all modes of generation, from breathing to coughing, micro-droplets far outnumber large droplets.
Outside air, air exchange and high filter efficiency reduce the risk of transmission
Dilution of indoor air with outside air, the removal of polluted indoor air as exhaust air and, in the case of recirculated air, filtration, reduce the risk of transmission by airborne pathogens by decreasing the concentration of pathogens in the air. Studies at the Hermann Rietschel Institute (TU Berlin) have shown that the CO2 concentration is a good indicator of ventilation system efficiency in relation to the number of people present as well as, indirectly, a good indicator of the virus concentration and the risk of infection in closed rooms.
Even if the indoor air is exchanged several times per hour, low virus concentrations remain in the room for considerably longer than one hour. The risk of transmission therefore also depends on the length of time for which Covid-19 viruses remain infectious in the air and how many viruses it takes to infect a susceptible person. Human experiments with flu virus aerosols conducted in the 1960s showed that two to three flu viruses are sufficient for transmission. For SARS-CoV-2 and all other coronaviruses, this number is unknown. Genetic material from SARS-CoV-2 viruses has been found in numerous cases in the indoor air of hospitals where Covid-19 patients are being treated. These results suggest that the number of viruses in well-ventilated rooms without massive accumulation is in the one- to two-digit range per m³ of indoor air. Since an adult breathes in 14 to 18 m³ of indoor air per day during physical exertion, even a few infectious viruses per m³ pose a relevant risk of infection. Due to the extremely demanding detection technique, the detection of infectious SARS-CoV-2 viruses in indoor air has failed so far, with only a few viruses being found per m³ of indoor air.
Humidity, temperature and solar radiation determine SARS-CoV-2 viruses’ duration of infectivity
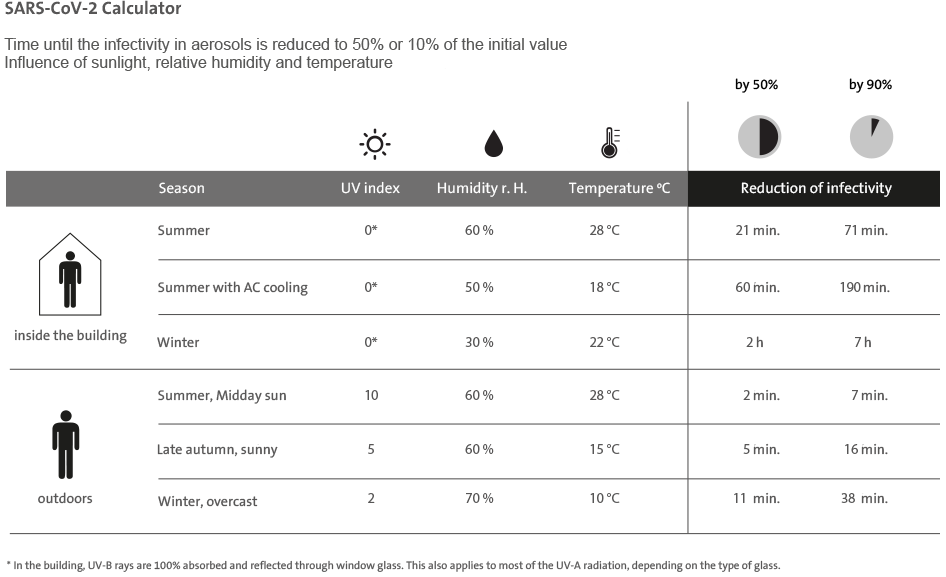
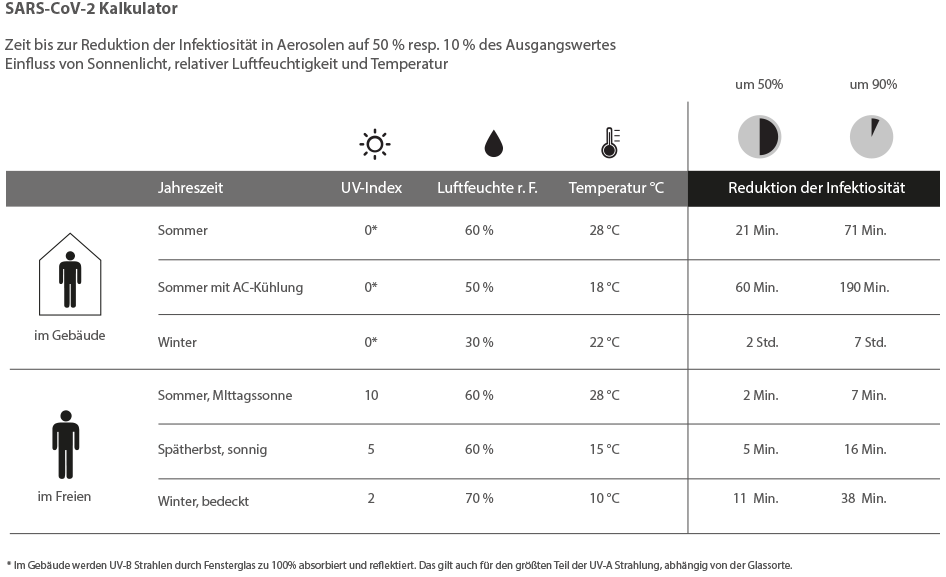
The environmental factors of indoor climate and sunlight influence the risk of transmission, as they determine the duration of infectivity of emitted viruses in the air and on surfaces. Since indoor temperature only varies within a narrow comfort range and sunlight is completely absent in buildings with closed windows, humidity is the critical factor determining the duration of infectivity of SARS-CoV-2 viruses in the air and on surfaces. The US National Biodefense Analysis and Countermeasures Center has published two SARS-CoV-2 calculators based on two studies and ongoing experiments. The calculators can be used to estimate how environmental factors influence the duration of infectivity of Covid-19 viruses in aerosols and on surfaces. Selected results for common indoor and outdoor climatic situations as well as links to the studies and the calculators are provided in the table overleaf. SARS-CoV-2 viruses are most effectively deactivated by the ultraviolet component of solar radiation (UV-A and UV-B), which unfortunately is almost 100% absorbed and reflected by most window glass. Therefore, in the comfort range of temperature, the duration of infectivity of the viruses is determined almost exclusively by the humidity in buildings.
Allowing the relative humidity in our buildings to drop to percentages in the low twenties during the heating season means no deactivation of the SARS-CoV-2 viruses will take place at all. Raising the humidity from 30% to 60% shortens the time to deactivation of 50% and 90% of the viruses from 2 to 0.5 hours and from 7 to 1.5 hours, respectively (see table).