Study by Wan Yang
Humidity has been linked to seasonal influenza. However, the mechanisms underlying this relationship remain unclear. There is no consistent explanation for the transmission patterns of influenza that apply to both temperate and tropical regions. The aim of this study was to determine the relationship between humidity and the viability of influenza A virus (IAV) during transmission between hosts and to explain the underlying mechanisms. We measured the viability of IAV in droplets composed of various model media selected to assess the effects of salts and proteins in respiratory fluid and human mucus at relative humidities (RH) ranging from 17% to 100 % isolate. In all media and slime, viability was highest when the relative humidity was either near 100% or below 50%.
When the relative humidity decreased from 84% to 50%, the relationship between viability and relative humidity depended on the composition of the droplets: viability decreased in saline, did not change significantly in protein-fortified solutions, and increased dramatically in mucus. In addition, virus breakdown increased linearly with salt concentration in salt solutions, but not when they were supplemented with proteins. There appear to be three regimes of IAV viability in droplets, defined by humidity: depending on physiological conditions (100% RH) with high viability, concentrated conditions (50% to near 100% RH) with lower viability on the composition of the media and dry conditions (50% RH) with high viability. This paradigm could help resolve conflicting results in the literature on the relationship between IAV viability in aerosols and moisture, and results in human mucus could help explain the seasonality of influenza in different regions.
Introduction
Influenza has different transmission patterns around the world. In temperate regions, the incidence of influenza is in winter [1,2], while in some tropical regions the incidence of the disease coincides with the rainy season [3-5]. These patterns have sparked a keen interest in uncovering the mechanisms behind them. However, despite almost a century of research, there is no consistent explanation [6,7]. Humidity has been identified as a factor influencing influenza seasonality [8,9]. Previous studies have linked the high incidence of influenza in temperate regions to low winter humidity [10-12]. This relationship is supported by laboratory studies which indicate that the influenza A virus (IAV) survives better at low relative humidity (RH) [8,13-15].
However, some important questions remain unanswered. First, the association between high incidence of influenza and low humidity cannot explain the increased influenza activity in some tropical areas during the rainy season when the humidity is at its maximum. Second, the results at medium to high (50% to 90%) relative humidity were discordant [7], although laboratory studies consistently showed a high survival rate for IAV at low relative humidity (50%). Of the four most cited studies, Hemmes et al. [8] and Harper [13] (hereinafter referred to as H&H) found higher inactivation rates both at medium and at high relative humidity, while Shechmeister [15] and Schaffer et al. [14] (hereinafter referred to as S&S) reported the highest inactivation rates at medium relative humidity and moderate at high relative humidity. The relationship between the viability of IAV in droplets in air and the relative humidity in the environment remains poorly defined and poorly understood.
Another unanswered question concerns the mechanism by which air humidity could influence the IAV in airborne respiratory droplets [9]. After being released from the respiratory tract, where the relative humidity is around 100%, a respiratory droplet shrinks by 40 to 50% in diameter at a relative humidity below 90% due to evaporation [16-18]. As a result, the concentrations of solutes in the droplet increase up to 15 times and solutes such as salts (e.g. sodium chloride (NaCl)), which are harmless in physiological concentrations, can become harmful to the virus. For example, Vogel IAV has been reported to be less stable at salinities greater than 25 g / L [19]. The evaporation results in changes in the microenvironment of IAV in droplets that can affect the viability of the virus; the toxic effect of dissolved substances can be increased at lower relative humidity due to higher concentrations resulting from greater water loss. However, respiratory droplets also contain a large number of proteins [20,21], and their interactions with salts at different relative humidity levels can complicate this picture under natural conditions. We hypothesize that humidity affects the survival of IAV in a droplet by controlling the amount of evaporation and thus solute concentrations in the droplet, and that solute concentrations in the droplet determine the relationship between relative humidity and the viability of the IAV define.
We developed a simple experiment to test the effects of salts and proteins on the viability of IAV and, for the first time, to determine its relationship to the relative humidity in human mucus. Our results solve the above mentioned discrepancy in the literature. Based on these results, we propose a mechanistic explanation for the dependence of IAV survival on humidity and influenza transmission patterns in temperate and tropical regions.
Materials and methods
Ethics statement
The collection and use of human slime has been approved by the Virginia Tech Institutional Review Board. The ethics committee did not need approval for this protocol.
Cells and virus
Madin-Darby canine kidney (MDCK) cells were maintained in Dulbecco's modified Adler medium (DMEM) supplemented with 5% fetal calf serum (FCS). The herd of IAV A / PR / 8/34 (H1N1) was created with a plaque-purified strain [22] in ten-day-old specific, pathogen-free embryonated chicken eggs. Virus stocks were stored as aliquots of allantoic fluid from infected embryos at 280 ° C until used. The titer of the virus stock was determined to be 1.786108 ml (TCID50) in the median of the infectious tissue culture21. All virus titration experiments were performed in MDCK cells.
Slime sample
A mucus sample was collected from a one month old infant in March 2011. The slime sample was dried in a vial and dissolved by dissolving in MilliQ water (5% w / v). In order to preserve the structure of the mucus, we first tried to sterilize the sample of mucus by passing it through a filter with a pore size of 0.45 mm. The sample was not filterable, which indicates its large molecular size. The reconstructed mucus was thus sterilized by heating at 65 ° C. for 30 minutes and checked for potential IAV contamination by the TCID50 test. No IAV was detected and the sample was stored at 4 ° C until used.
Control of the relative humidity in a desiccator
Two petri dishes filled with 20 ml of saline solution (either potassium acetate, potassium carbonate, cobalt (II) chloride or potassium chloride) or double distilled water were placed in a desiccator [23, 24]. The air circulation inside the desiccator was improved by a fan in order to accelerate the establishment of an equilibrium humidity between the saline solution and the air inside the desiccator. Before each experiment began, the desiccator was conditioned to the desired relative humidity. The desiccator had to be opened briefly to insert the samples and the system restored equilibrium within ten minutes. The actual r. F. and the temperature inside the desiccator were recorded with a temperature / humidity logger (OM-73, Omega Engineering, Inc., USA) at one minute intervals during sampling. Relative humidities tested in model media included 17.5 ± 1.0%, 27.6 ± 0.9%, 42.0 ± 0.8%, 44.1 ± 1.2%, 50.2 ± 0.7% , 59.5 ± 1.1%, 76.1 ± 0.7%, 84.1 ± 0.8% and 98.9 ± 0.4%. Relative humidities tested in slime samples contained 26.7 ± 0.8%, 40.3 ± 1.1%, 48.0 ± 1.2%, 52.0 ± 0.9%, 60.8 ± 1.1% , 72.2 ± 1.2%, 83.9 ± 0.4% and 99.1 ± 0.4%.
Exposure of IAV in droplets to various relative humidities
We exposed IAV in droplets at room temperature (20-24 ° C) to specific relative humidities in the range of 17% to 100%. The droplets consisted of four different types of media selected to isolate the effects of salts and / or proteins on viability or on mucus. PBS and DMEM were used as replacements for media containing inorganic salts in physiological amounts but no or negligible amounts of proteins. The third and fourth media types were PBS and DMEM supplemented with 5% FCS, a source of protein. 10 µL of PR / 8 IAV stock solution was added to 90 µL of either PBS, PBS + 5% FCS, DMEM, DMEM + 5% FCS, or mucilage to make spiking solutions. The spiking solutions were dispensed onto a 12-well cell culture plate, 1 μL per droplet, 10 droplets per well, and 3 replicates (i.e. 3 wells) for each medium.
The plate was immediately placed in the desiccator and at a specific r. F. Incubated at room temperature for three hours for model media and two hours for mucus. At the end of the period, the virus was collected in each well with 1 μL DMEM supplemented with 1 μg / L TPCK trypsin (collection medium) by pipetting the medium 10 times to flush the virus from the well. The spiking solutions were stored on ice during the incubation period and 10 μL of each spiking solution was supplemented with 990 μL collection medium for use as a control. The samples and the corresponding controls were titrated at the same time by the TCID50 assay either immediately after collection or stored at -80 ° C until tested. Media used in influenza A virus viability studies versus RH.
Observation of the transformation of droplets under varying relative humidity values
Droplets of PBS, PBS + 5% FCS, DMEM or DMEM + 5% FCS (all without addition of IAV) in 1 μL volumes were distributed on a 12-well cell culture plate and, as described above, incubated under various relative humidity values . Plates were removed from the incubator and immediately observed under an inverted light microscope (100X).
Photos were taken by a camera connected to the microscope. To determine the time it takes a droplet of 1 μL to dry out, droplets of PBS, PBS + 5% FCS, DMEM or DMEM + 5% FCS were spread on a glass slide under the microscope and continuously observed until the drop crystallized. The ambient humidity was 49.4 ± 0.2% in the microscope room.
Calculation of the viral decay rate
The percent viability was calculated as viability = N
t/N
0 x 100%, where N
t and N
0 are the final and initial titers of the virus, respectively.
The logarithmic decay rate was calculated as log decay = log
10(N
t/N
0). N
t was set to 1 for negative samples to avoid division by 0.
Estimation of the concentration of dissolved substances in equilibrium
The molality of NaCl in the resulting droplet at a specific RH was calculated using the Microsoft solver tool according to an empirical relationship [25]:
where m is the molality of NaCl (mol (kg water) -1). The concentration of NaCl was then calculated based on m:
Cs = mMs/mvs + 1
where Cs is the solute concentration in equilibrium; Ms is the molecular weight of NaCl (58.44 g mol - 1); vs is the molar volume of NaCl (2.761022 L mol - 1); and the number 1 in the denominator represents the volume of 1 kg of water, i.e. H. 1 L.
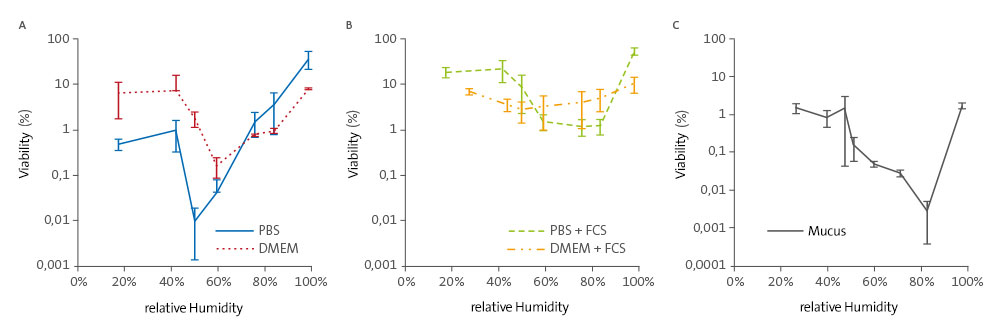
Figure 1. Relationship between relative humidity and viability of the IAV in (A) media with mainly salts,
(B) media with salts plus proteins; and (C) mucus. Error bars indicate standard deviations.
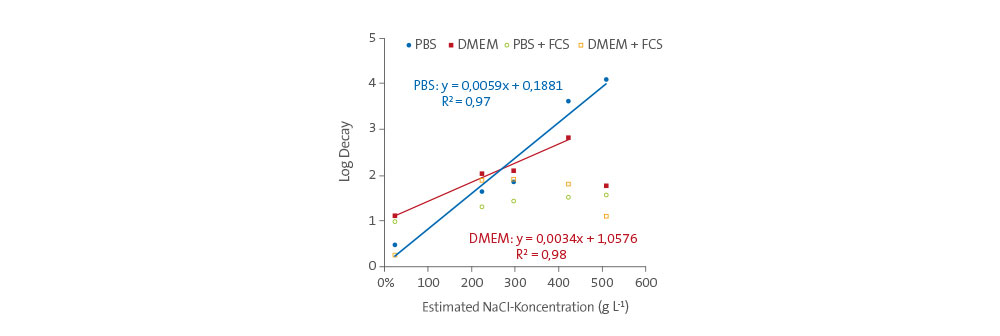
Figure 2. Virus disintegration over 3 hours versus the NaCl concentration in droplets,
which consist of four media types.
Results
IAV Viability in Model Media vs. Relative Humidity
As shown in Figures 1A and 1B, the IAV viability in four model media containing different combinations of salts and proteins were at extremely high (ca 100%) and low (< 50%) r. F. and minimally at medium (50 to 84%) R. F. highest. At 100% r. F. viability ranged from 8% to 57%, namely 36 ± 15% in PBS, 7.8 ± 0.27% in DMEM, 11 ± 4.1% in PBS + FCS and 57 ± 11% in DMEM + FCS of the introduced virus. At 84% r. F. life skills were much lower (1-5%) but were of the same order of magnitude in all four media.
With relative humidity between 50% and 84%, viability trends diverged dramatically depending on whether the media contained proteins or not. The viability in PBS decreased with decreasing r. F. and reached a minimum at 50% relative humidity. In DMEM the trend was similar, but the minimum occurred at 60% humidity (Fig. 1A).
In contrast, the viability in PBS + FCS did not change significantly over this humidity range and in DMEM + FCS the viability increased with decreasing r. F. easy to (Fig. 1B). At relative humidities below 50%, viability in all types of media was higher than that of medium r. F. although the viability in PBS alone was significantly lower than the three other media, possibly due to the lack of proteins.
We repeated the experiment to confirm these results. The percent viabilities recovered varied slightly, but the trends in profitability versus r. F. were similar.
IAV viability in mucus versus relative humidity
We tested the changes in the viability of IAVs invaded human mucus at RH levels of 26 to 100%. As shown in Fig. 1C, r was 100%. F. IAV viability only 1.7 ± 0.26%, an order of magnitude lower than in model media. The finding that the viability at this extremely high r. F. was highest, agreed with results in other media. At a relative humidity between 50% and 84%, the viability decreased with decreasing r. F. dramatically too. Only 0.0027 ± 0.0023% was recovered at 84% relative humidity compared to 1.5 ± 1.4% recovered at 48% relative humidity, a decrease of more than two orders of magnitude. At r. F. Below 48%, the habitability has leveled off and remains at around 1%. We repeated the experiment at four (27%, 60%, 84% and 99%) of the six relative humidities and the resulting vivities followed the same trend as shown in Figure 1C. With spike titers of 5.1 ± 2.6x104 TCID50, no viable IAV was found in 5 of 9 samples at 84% r. F. proven.
Relationship between virus decay and salt concentrations
The relationship between the disintegration rates of the viruses and the salt concentrations in the droplets is shown in Fig. 2. The four media used in this study and the mucus sample contained several types of salts. However, since NaCl was the main salt in all media and in the mucus, we estimated the total concentrations of salts in the droplets at equilibrium as equivalent amounts of NaCl; Concentrations were estimated empirically [25]. The concentration of NaCl in a droplet is given by r. F. connected; However, as shown by the polynomial function in Eq. 3 the correlation is not simply linear.
The virus degradation rate in PBS droplets increases linearly with the NaCl concentration in the range of 25-510 g / L, corresponding to 99-50% r. F. (R2 = 0.97). The concentrations are lower at high relative humidity, since the evaporation is lower and vice versa. In a similar way, the virus breakdown rate in DMEM droplets increases linearly with the NaCl concentration up to 420 g / L, corresponding to 60% r. F. (R2 = 0.98). In contrast, the virus disintegration rates in media containing FCS remain constant regardless of the NaCl concentration.
Efflorescence
At a relative humidity below 50%, the relationship between IAV decay rates and NaCl concentrations is no longer valid. NaCl reaches its solubility in a droplet (310 g / L) at 75% r. F., and evaporation creates a supersaturated solution at r. F. & lt; 75%. The NaCl concentration can rise up to 580 g / L before the droplet crystallizes [25,26]. The critical relative humidity at which a droplet crystallizes is called the efflorescence RH (ERH) and depends on the composition and size of the droplet [27].
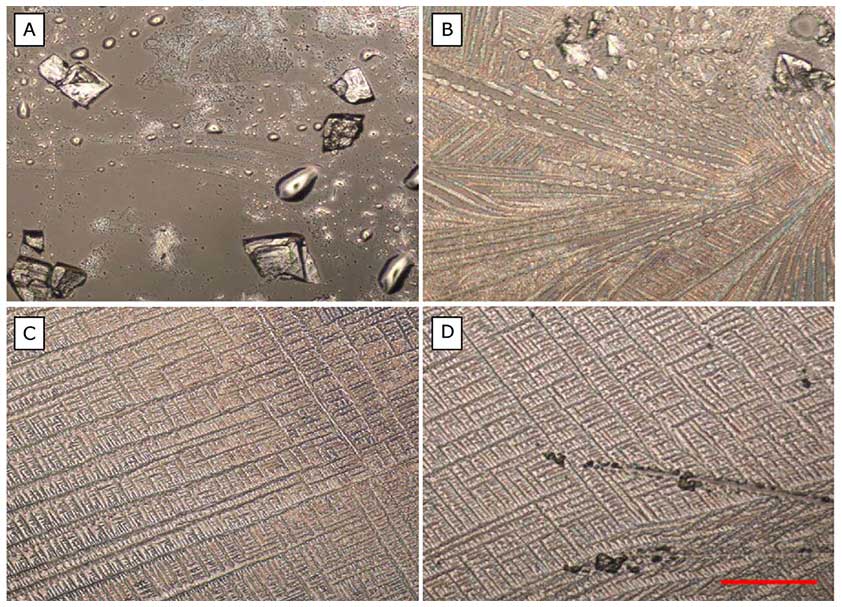
Figure 3: Crystals of the four media: (A) PBS, (B) PBS + FCS, (C) DMEM,
(D) DMEM + FCS. Light microscope, magnified 100 times; Scale bar = 20 μm.
We observed the droplets of each medium under a microscope immediately after incubation at various relative humidities and found that r. F. & gt; 60% no crystals while droplets of all media at r. F. just under 50% crystallized (Figure 3). Crystallization occurred within ten minutes. Crystallization in DMEM, possibly at a lower NaCl concentration (correspondingly higher RH) than in PBS, due to a different ERH of the media, could result in the lower rate of decrease in DMEM at a concentration of 510 g / L (50% RH) .) explain.
Knowing the ERH of each medium would further support this idea, but the ERH of a solution is difficult to calculate and can only be accurately measured through specialized laboratory experiments [27].
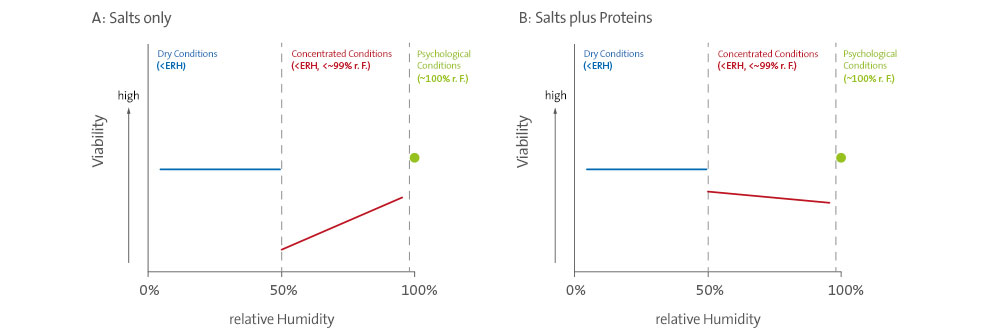
Figure 4. Hypothetical relationship between relative humidity and the viability of the IAV in (A) droplets,
containing salts only, and (B) droplets containing salts and proteins.
Discussion
Hypothesis explaining the relationship between r. F. and viability in laboratory studies
We postulate that there are three regimes that determine the viability of IAV in droplets, defined by ambient humidity and shown in Fig. 4: (1) Physiological conditions (~ 99 to 100% RH) at which the Solute concentrations for which IAV are harmless and viability is maintained, (2) concentrated conditions (50 to 99% RH) where evaporation leads to elevated salt concentrations that can be harmful to the virus, and (3) dry conditions (< 50% RH) where the solutes crystallize, all water is lost and the viability of the IAV is maintained.
In a salt droplet, the increased salt concentrations resulting from evaporation are likely to be toxic to the virus, but such deleterious effects would be eliminated if the solution crystallized. Therefore, the minimum viability would be expected at a relative humidity just above the relative humidity of the salts contained in the droplet, when water is still present and the concentrations of the solutes are at a maximum. The relationship between relative humidity and IAV viability in a salt droplet would therefore be similar to that shown in Figure 4A. However, the presence of proteins in the droplet can alter this relationship.
It is possible that the interaction between proteins, salts, and the virus mitigates the adverse effects of salts in concentrated conditions. Therefore, the virus would maintain high viability under physiological and dry conditions and moderate viability under concentrated conditions in a droplet composed of both salts and proteins (Figure 4B). Indeed, the lower the r. F. increase, as we found with DMEM + FCS and mucus, possibly due to protection by proteins at elevated concentrations [28, 29].
A study on the Langat virus supports our hypothesis. Benbough [30] reported similar V-shaped curves of viability versus r. F. for Langat virus in aerosols, which consist of saline solutions. Of the four relative humidities tested (i.e. ~ 25%, 50%, 70% and 95%), the minimum vivities were ~ 1% in NaCl and ~ 10% in KCl, both at ~ 50% RH. F. and zero in LiCl at r. F. & lt; 50%. Thus, the minimal viability of Langat virus occurred in aerosols consisting of a NaCl solution at a relative humidity close to the ERH of NaCl (i.e. 43 ± 3%) [27]. KCl has an ERH of 59% [27], and this r. F. has not been tested so it is not known whether the virus' viability in this r. F. would have been lower. The ERH of LiCl, if it exists, is outside the range of relative humidities tested; the relative humidity in the resolution is ~ 11% [24].
Explanation for conflicting results in the literature
Upon reviewing the four studies above (H&H versus S&S), we found that the media used to make airborne droplets with IAV differed. All media contained some salts; those in H & amp; However, H contained significantly more proteins than those in S & amp; S. We therefore suspect that the conflicting results between S & amp; S and H & amp; H due to the different protein content of the media used in these studies. Our results with model media confirm this hypothesis: the trends in viability to relative humidity in media with mainly salts (S&S and this study) are similar to that shown in Figure 4A, while those in media with salts and proteins (H&H and this study) are similar to Figure 4B.
Figure 2. Virus disintegration over 3 hours versus NaCl concentration in droplets consisting of four media types.
Figure 3. Crystals of the four media: (A) PBS, (B) PBS + FCS, (C) DMEM, (D) DMEM + FCS. Light microscope, magnified 100 times; Scale bar = 20 μm.
Figure 4. Hypothetical relationship between relative humidity and IAV viability in (A) droplets containing only salts and (B) droplets containing salts and proteins.
We have shown that virus disintegration correlates with the salt concentration in salt droplets, which is controlled by evaporation through relative humidity (Figure 2). Earlier studies based on experiments in bulk salt solutions at concentrations up to saturation could not demonstrate such a correlation [31]. The supersaturated conditions to which the virus is exposed in aerosols cannot be achieved in mass media, and so the phenomenon observed here can only be demonstrated by methods that enable supersaturation. The combination of greatly increased salt concentrations at medium relative humidity and salt crystallization at the ERH can explain the trends observed in the two media, which contain mostly salts (i.e., PBS and DMEM), and in S&S.
The relative humidity, which corresponds to the maximum decay rate, can differ between the media, possibly due to different ERHs for media of different composition [27]. The minimum viability was between 40-70% r. F., mainly at about 50% in Schaffer et al. [14] and 58-60% in Shechmeister. [15] For comparison, we found a minimum viability of 50% in PBS and 60% in DMEM.
Like H&H, we found proteins to have a protective effect on IAV under concentrated conditions at medium r. F., although the reasons for this are still unknown. One possibility is that proteins in aerosol droplets can accumulate around viruses due to mutual hydrophobicity and offer a certain protection against concentrated salts. Although this hypothesis is very speculative, it is supported by the fact that mucin glycoproteins normally act as a barricade against potential pathogens, including viruses and bacteria, through specific or non-specific binding [28, 29].
Relationship in slime
Respiratory tract mucus is an intricate combination of water (95%), inorganic salts (1%), and various macromolecular organic compounds including glycoproteins (i.e. mucins) and lipids [20, 21, 32]. It has been shown to be IAV at lower r. F. protects [33, 34]. However, the relationship between the viability of IAV in mucus and relative humidity is not yet completely clear. We first carried out experiments with mucin extracts from pig stomach (type II, Sigma-Aldrich). The results indicated that the IAV infection was blocked, probably due to the bound sialic acid on the mucin. Similarly, glycans on human mucus could prevent IAV attachment to the cell in the TCID50 assay. However, such an effect was not significant according to our experiment. The titer of IAV spiked into the human mucus sample was 5.1 ± 2.6x107 TCID50 ml-1 after being kept on ice for two hours with a peak titer of 1.78x108 TCID50 ml-1. In addition, the results of reporting in mucus samples as the ratio of viability restored after incubation at a certain relative humidity to the original viability, both of which were tested in the mucus, should assess the possible blocking effect of glycans on the mucus. Therefore, the results reported here reflect the effect of relative humidity.
In agreement with the literature [33,34] we found higher viability at low relative humidities (< 50%). Finding that IAV survived best at 100% relative humidity, a condition that has not been previously investigated, helps understand the virus' response to varying r. F. to complete.
The relationship in mucus bears some resemblance to that in media with salts and proteins, especially DMEM + FCS (i.e. higher vivities at 100% RH or RH < 50% and much lower at medium RH. in the range from 50% to 84%). However, the viability to humidity in the slime was much more sensitive than in synthetic model media. A small change in relative humidity from 48% to 52% reduced viability 10-fold and viability at 84% relative humidity was> 500 times lower than at 48% relative humidity. For comparison, the viability in the model media varied by only one order of magnitude in the same humidity range, which is in agreement with earlier studies [8, 13].
Therefore, r. F. Have a greater effect on the survival of IAV in mucus than has been shown in previous studies with synthetic media. These results highlight the potential impact of relative humidity on the survival of the virus in its natural aerosol carrier during transmission.
Implications for Influenza Transmission Patterns
Many mechanisms have been proposed to explain the seasonality of influenza, including (1) environmental and climatic factors (e.g. temperature, relative or absolute humidity, and sun intensity), (2) host behavioral changes (e.g. school schedule and increased visitor numbers in winter or during the rainy season) and (3) fluctuations in the host's immune competence (e.g. vitamin D level and melatonin level) [7.35]. A current review by Tamerius et al. [7] assesses the feasibility of various mechanisms and concludes that the central issues of influenza seasonality remain unsolved. Our study focused on the influence of moisture and we carried out all experiments at room temperature. In indoor spaces, where infection is more likely due to the much longer time spent there and the greater spatial density of potential hosts, the temperature tends to drop in a narrow range around 20 ° C. With this limitation, we were unable to distinguish between the effects of relative and absolute humidity.
Our findings in human mucus could help explain, at least in part, the transmission patterns of influenza. In the temperate regions, the warming in winter reduces the relative humidity indoors to low values, usually 40% [36,37]. Low relative humidity not only helps maintain IAV viability, it also allows IAV carrier aerosols to remain in the air longer due to their smaller size and lower settling rates resulting from increased evaporation [16]. For example, the transmission of influenza in temperate regions in winter could be intensified, especially via the aerosol route. In tropical regions, high temperatures can suppress transmission, especially via the aerosol route [38, 39]. However, lower temperatures and almost saturated humidity during the rainy season offer the possibility of transferring large droplets or very small aerosols via various mechanisms. Large droplets would settle faster due to gravity, since they do not shrink as much at 100% relative humidity (only 93% of their original diameter at 99% r. F. and 76% at 98% r. F. [16]). Once deposited on a surface, they can serve as a reservoir for contract transfer [39,40] since IAV, as shown in this study, is well preserved at 100% relative humidity. On the other hand, submicron aerosols such as those exhaled in human breath [41] would remain in the air, and thanks to the lower temperatures and relative humidities suitable for survival, aerosol transmission through these submicron droplets could still be possible be effective.
Limitation and directions for future study
In this study, droplets of 1 μL were used instead of smaller aerosols [42] to simulate the interplay of moisture, droplet evaporation, solute concentrations in the droplet, and virus viability. It takes ~ 10 minutes for such droplets at ~ 50% r. F. Dry out completely, considerably longer than with much smaller droplets (e.g. < 1 s for a respiratory droplet with a diameter of 20 μm [17]). The legitimacy of extrapolating our results to aerosols expelled from the human respiratory tract therefore depends on whether the evaporation dynamics is critical to IAV decay. Our results in model media are comparable to those in aerosols [8,13]. Harper [13] recovered 66–126% of the IAV in aerosols 1 s after spraying when evaporation was complete. The high recovery rates show that the effect of the evaporation process itself on virus disintegration is negligible.
While this was critical, such an effect was controlled by comparing the virus breakdown in the same type of medium with the relative humidity, since all droplets had a similar evaporation rate. However, checking these results in aerosols is justified.
This study proposes a new mechanistic basis for the effect of relative humidity on the viability of IAV in droplets. However, it does not address the mechanism by which salts affect IAV viability at the molecular level, nor does it explain how the presence of proteins alters the relationship. In addition, the relationship in mucus was slightly different from the relationship observed in the model media. Given the complex composition and unique nature of mucus, mechanisms that control the relationship in mucus may differ from those in model media.
Conclusions
This study reports new data on the response of IAV in droplets of model media to varying relative humidities, including extreme conditions that have never been studied and, for the first time, the relationship between IAV viability in human mucus and humidity over a wide range of relative humidity. The results suggest that there are three regimes of IAV viability defined by relative humidity. We provide a mechanistic explanation for these regimes based on droplet evaporation, a subsequent increase in solute concentrations in the droplet and their effect on the virus. Our theory also explains the conflicting results in the literature on the viability of IAV in droplets [8,13-15]. We also outline a new perspective on the dependence of IAV transmission on humidity, which offers a possible explanation for the seasonal occurrence of influenza in different regions.


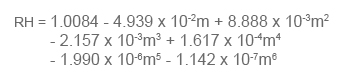
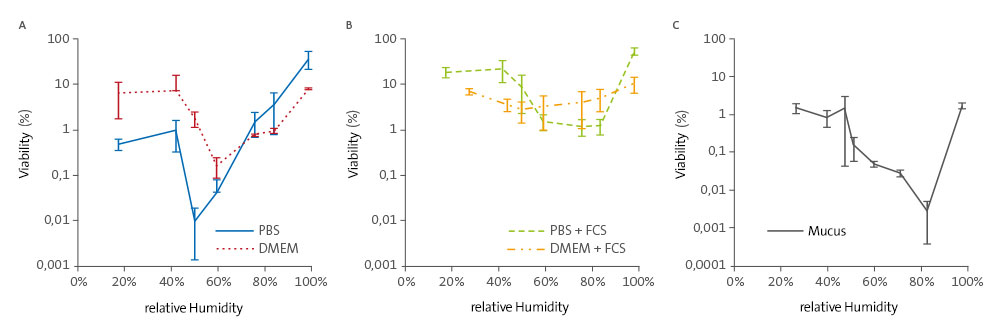 Figure 1. Relationship between relative humidity and viability of the IAV in (A) media with mainly salts,
Figure 1. Relationship between relative humidity and viability of the IAV in (A) media with mainly salts, 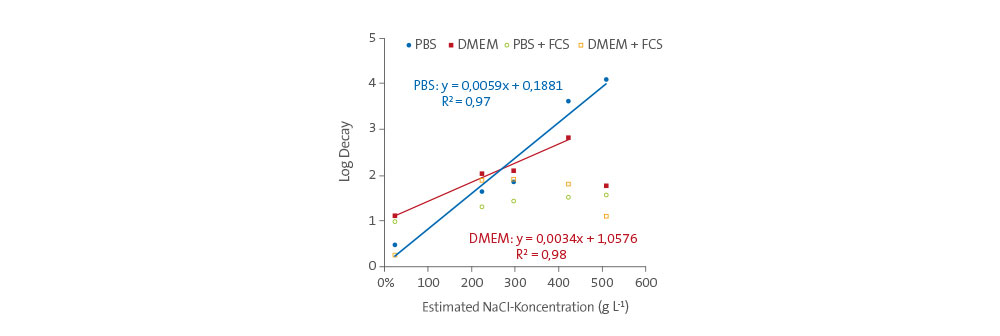 Figure 2. Virus disintegration over 3 hours versus the NaCl concentration in droplets,
Figure 2. Virus disintegration over 3 hours versus the NaCl concentration in droplets,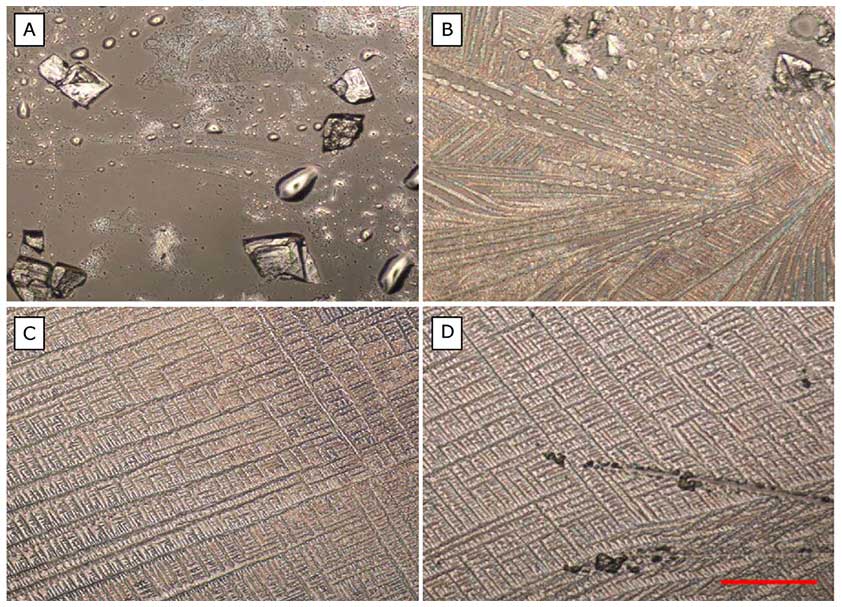 Figure 3: Crystals of the four media: (A) PBS, (B) PBS + FCS, (C) DMEM,
Figure 3: Crystals of the four media: (A) PBS, (B) PBS + FCS, (C) DMEM,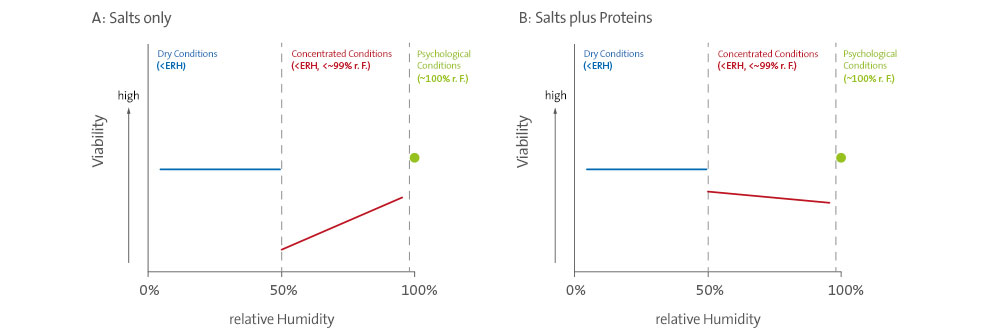 Figure 4. Hypothetical relationship between relative humidity and the viability of the IAV in (A) droplets,
Figure 4. Hypothetical relationship between relative humidity and the viability of the IAV in (A) droplets,