Study by Anthony V. Arundel
A review of the health effects of relative humidity in indoor environments suggests that relative humidity can affect the incidence ofrespiratory infections and allergies. Experimental studies on airbome-transmitted infectious bacteria and viruses have shown that the survival or infectivity of these organisms is minimized by exposure to relative humidities between 40 and 70%. Nine epidemiological studies examined the relationship between the number of respiratory infections or absenteeism and the relative humidity of the office, residence, or school. The incidence of absenteeism or respiratory infections was found to be lower among people working or living in environments with mid-range versus low or high relative humidities. The indoor size of allergenic mite and fungal populations is directly dependent upon the relative humidity. Mite populations are minimized when the relative humidity is below 50% and reach a maximum size at 80% relative humidity. Most species of fungi cannot grow unless the relative humidity exceeds 60%. Relative humidity also affects the rate of offgassing of formaldehyde from indoor building materials, the rate of formation of acids and salts from sulfur and nitrogen dioxide, and the rate of formation of ozone. The influence of relative humidity on the abundance of allergens, pathogens, and noxious chemicals suggests that indoor relative humidity levels should be considered as a factor of indoor air quality.
The majority of adverse health effects caused by relative humidity would be minimized by maintaining indoor levels between 40 and 60%. This would require humidiftcation during winter in areas with cold winter climates. Humidiftcation should preferably use evaporative or steam humidifters, as cool mist humidifters can disseminate aerosols contaminated with allergens.
Introduction
Over the last 15 years, the quality of air in indoor environments such as houses, apartments, and offices has been extensively investigated. Field studies have frequently found undesirably high levels of known respiratory irritants such as nitrogen and sulfur dioxides, hydrocarbons, and particulates (1) and known or suspected carcinogens such as asbestos, radon, some particulates, and formaldehyde (2). In many cases, high indoor levels of contaminants have been traced to indoor building materials, furnishings, appliances, and human activities. Indoor contaminant levels can also be exacerbated in tightly sealed energy conserving buildings with low fresh air ventilation rates. Either reducing the sources of pollutants or increasing ventilation rates, or both, can be used to reduce or eliminate the levels of these contaminants.
Water vapor, usually measured as relative humidity or the percentage of water vapor held by the air compared to the saturation level, is not usually considered to be an indoor contaminant or a cause of health problems. In fact, some level of humidity is necessary for comfort. On the other band, the relative humidity of indoor environments ( over the range of normal indoor temperatures of 19 to 27°C, has both direct and indirect effects on health and comfort. The direct effects are the result of the effect of relative humidity on physiological processes, whereas the indirect effects result from the impact of humidity on pathogenic organisms or chemicals.
This review is primarily concerned with the indirect health effects of relative humidity, which are more complex than the direct health effects and of greater public health significance. However, it is worthwhile to briefly discuss some of the direct health effects, as these effects often lead to solutions (such as humidification) which may in turn indirectly affect health.
Direct Health Effects
Both very low or high relative humidities may cause some physical discomfort, as the relative humidity of the air directly affects temperature perception (3). Extremely low (below 20%) relative humidities may also cause eye irritation (4,5) and moderate to high levels of humidity have been shown to reduce the severity of asthma (6). Several reports, apparently based on the experience of physicians with patients who complained of dryness of the nose and throat during low relative humidities, have also argued that indoor relative humidities should be kept above 30 to 40% in order to prevent drying of the mucous membranes and to maintain adequate nasal mucus transport and ciliary activity (7-10). These known or suspected adverse effects oflow relative humidity have led to the widespread use of humidifiers in areas where cold winters lead to low indoor humidities. However, there is little experimental evidence to indicate that the mucous membranes of healthy individuals are adversely affected by low relative humidities (11), though there is also little evidence to the contrary. The only experimental investigation of this problem failed to find a relationship between low humidity and dehydration of the mucous membranes. Andersen et al. (12) examined the posterior nasal mucociliary flow of eight healthy male subjects between 21 and 26 years of age exposed to 9% relative humidity in a climate chamber for 3 days. The mucosal flow actually increased after 3 days of exposure at 23°C compared to the control period of exposure to 50% relative humidity at the same temperature. There were few complaints of skin or membrane dryness. lt is also possible that considerably longer periods of exposure to low relative humidities are required to cause drying of the mucosal membranes, or that an interaction between low relative humidity and dusts or pollens may irritate mucous membranes.
Relative humidity may, however, directly affect the mucous membranes of individuals with bronchial constriction, rhinitis, or cold and influenza related symptoms. One study found that the humidification capacity of the anterior nose was reduced during rhinitis (13), and another study found a small decrease in the humidifying capacity of the nose among four subjects with atrophic rhinitis compared to 22 normal subjects (14). Relative humidity may also affect bronchial mucus if nasal congestion leads to breathing throngh the mouth. An in vitro study on the effect of relative humidity on the viscosity of bronchial mucus found a twofold decrease in viscosity when the relative humidity was 100% versus 60% (15). Water mist, produced intentionally or accidentally by several types of humidifiers, may be partly responsible for the beneficial effects of humidification, as mists have been found to reduce mucus viscosity (16) and to reduce the incidence of upper respiratory infections, cough, and rhinitis among children with recurrent upper respiratory illness (11).
Relative humidity also has an important adverse direct effect on health when high humidities are combined with high temperatures. This combination reduces the rate of evaporative cooling of the body and can cause considerable discomfort or lead to heat stroke, exhaustion, and possibly death.
lndirect Health Effects
Case reports and epidemiological studies suggest that relative humidity and humidification equipment can indirectly affect the incidence of allergies and infectious respiratory diseases. This effect is caused by the impact of both relative humidity and humidification equipment on the population growth and survival of infectious or allergenic organisms such as fungi, protozoans, mites, bacteria and viruses, as well as the probability of effective contact (exposure that results in disease or adverse symptoms) with these organisms. These indirect effects may partially account for the suspected relationship between respiratory infections and nose or throat irritation and relative humidity. In addition, relative humidity affects the concentration of noxious chemicals in the air by altering the rate of offgassing from building materials and by the reaction of water vapor with chemicals in the air. A review of the available data on the indirect health effects of relative humidity shows that these effects do not uniformly increase or decrease in frequency or severity with a change in relative humidity. Instead, for a given relative humidity, some adverse health effects can be at a maximum while others are at a minimum. The relative humidity range for minimizing as many adverse health effects as possible appears to lie between 40 and 60%. The evidence to support this optimum relative humidity range is presented below.
Relative Humidity and lnfectious Diseases
Diseases may be transmitted by airborne pathogens or through direct contact with pathogens living on hard surfaces such as furniture and plumbing fixtures, or by touching an infected person. Low relative humidities have been found to improve the survival of rhinoviruses and influenza virus (18) and human rotavirus (a cause of gastroenteritis) (19) on hard surfaces. However, the majority of illness caused by direct contact is thought to be due to contact with an infected person, and this latter mode of transmission is not known to be influenced by relative humidity. Conversely, experimental studies on the survival of pathogens in the air at various relative humidities and epidemiological studies on respiratory infections suggest that the indoor relative humidity can affect the incidence of infectious diseases transmitted by airborne pathogens.
The incidence of airborne-transmitted infectious diseases in the indoor environment is dependent upon six factors: the number of infected people producing contaminated aerosols, the number of susceptibles, the length of exposure, the ventilation rate, the settling rate of contaminated aerosols, and the survival of pathogens attached to aerosols (20).
The indoor relative humidity can affect two of these six factors: the settling rate of aerosols and the survival of airborne pathogens. Therefore, the importance of relative humidity as a determinant of the incidence of infections will depend upon the relative strength of these two factors compared to the other four. For example, relative humidity would probably have little or no effect on the incidence of infectious diseases in environments with very high fresh air ventilation rates.
Settling Rates of Aerosols
The amount of aerosols in a given volume of air is partially dependent upon the settling rates, which are a function of air movement and aerosol diameters (for aerosols with a diameter less than 100 µ.m). High settling rates reduce the abundance of aerosols which, in turn, reduce the probability of effective contact with aerosols contaminated with pathogenic substances.
Low relative humidities may increase the abundance of infective aerosols produced by coughing or exhaling. Rapid evaporation in dry air may cause the diameter of some aerosols to fall below the size limit for a particle to remain in suspension, whereas at higher relative humidities the same aerosol may reach the floor before sufficient evaporation occurs (21 ). Mid-range relative humidities (50-70%) have only a minor effect on aerosol size and subsequent settling rates (22). However, depending upon the initial composition and size of the aerosol, aerosol size may increase rapidly due to water absorption when the relative humidity exceeds 80 to 90%, leading to higher settling rates (23). In the United States and Canada, an increase in the abundance of suspended aerosols as a result of low relative humidities is more likely to have an effect on health than the decrease in aerosols during periods of very high relative humidity. Low indoor relative humidities are common in winter, when indoor air ventilation rates are 1ow and occupancy rates are high, whereas relative humidities above 80% are most likely to occur in summer, when better indoor ventilation through open windows and doors would reduce the possibility of effective contact with contaminated aerosols. Furthermore, the increase in air movement in summer would most likely cancel out the expected increase in settling rates due to an increase in aerosol size.
Experimental Studies on the Survival of Airborne Pathogens
Experimental studies have shown that relative humidity is an important factor in the survival of airborne pathogens. Relative humidity is thought to affect survival by altering the integrity ofthe cell wa11 or viral coat (24).
Bacteria
Bacteria that cause pneumonia, tuberculosis, Q fever, brucellosis, anthrax and Legionnaire‘s disease are air transmitted (25). However, little is known directly about the effect of relative humidity on the airborne survival or infectivity of pathogenic bacteria. On the other hand, the effect of relative humidity on nonpathogenic bacterial species such as E. coli has been extensively studied. In general, mid-range humidities (40-60%) are more lethal to airborne nonpathogenic bacteria than low or high humidities (24). A few studies on pathogenic or closely related bacterial species suggest that the response of pathogenic bacteria to relative humidity is similar to that of nonpathogenic varieties. Myca1plasma pneumoniae is an airborne-transmitted bacterium that can cause pneumonia or other severe respiratory infections. Tests on nonpathogenic Mycoplasma species indicate that the mycoplasms survive longer during exposure to either high or low relative humidities (26). A similar pattern of survival is found for a nonpathogenic species of Streptococcus (27). Serratia marcescens, an opportunistic bacterium that causes respiratory infections among patients in hospitals, is least viable during exposure to 50% RH and reaches maximum viability above 80% RH (28). High relative humidities above 70 to 80% are also preferred by Brucella suis (29) and by Staphywcoccus albus (30).
Viruses
The major airborne-transmitted viruses include influenza, measles, herpesvirus varicellae (the cause of chickenpox), rubella, the adenoviruses (the cause of acute respiratory disease with influenzalike symptoms), and the coxsackie viruses (the cause of some rashes and fevers) (20,31,32 ). Respiratory syncytial and para influenza viruses (both of which cause flulike symptoms) and rhinoviruses (the most frequent cause of the common cold syndrome) can also be transmitted by air, but the incidence of infections as a result of airborne transmission is thought to be very low compared to direct contact (20,33).
The effect of humidity on the viability of viruses depends on the viral molecular structure. High relative humidity tends to favor the survival of viruses composed entirely of nucleic acids and proteins, whereas lipid containing viruses prefer low relative humidities (34). The adenoviruses and the coxsackie viruses prefer relative humidities above 70% (35,36).
Measles, influenza, herpesvirus varicellae, and rubella viruses survive longer during exposure to relative humidities below 50%. Mass vaccination programs have reduced the public health significance of measles and rubella while infections due to adenovirus and coxsackie viruses normally occur at a low incidence rate in the population. Consequently, the influenza virus is the most important airborne-transmitted viral disease. Several laboratory studies have examined the relationship between relative humidity and influenza virus survival or infectivity. Hemmes et al. (37) and Harper (38) independently tested the viability of influenza virus attached to aerosols over a wide range of relative humidity. Both investigators sampled the air at various times after aerosol generation and tested for viral viability by inoculating live cell cultures with the air samples.
Hemmes found that viral inactivation rates increased sharply at relative humidities above 40%. Similarly, Harper found the percentage of viable influenza virus to decrease as the relative humidity was increased from 35% to 81%. Schulman and Kilbourne (39) directly tested the effect of relative humidity on the airborne transmission of influenza in mice. Uninfected mice were placed in cages adjacent to, but not touching, cages ofmice infected with influenza. The effect of relative humidity was determined after adjusting for the dilution effect of changes in ventilation. The infection rate decreased as the relative humidity
was increased from 47% to 70%.
The results of these experiments suggest that influenza infection rates are highest in environments with relative humidities below 40% and decrease rapidly as the relative humidity exceeds 40 to 50%. However, Lester (40) found that the rate of infection in mice exposed to aerosols containing influenza virus increased both below 40% and above 55% RH and was minimized during exposure to 55% RH. Schaffer et al. (41) found similar results. Aerosols of influenza virus cultivated in human cells were exposed to relative humidities between 20 and 80%. Viral survival was highest after exposure to 20%RH, fell to a minimum after exposure to relative humidities between 40 and 60%, and increased again after exposure to 70 to 80% RH, though the survival rate at 80% RH was less than the rate at 20% RH.
Consequently, it is possible that the infectivity of influenza virus shows an increase at both high and low relative humidities. Variations in the experimental results might have been due to different methods of preparing aerosols. In summary, the available data on bacterial and viral survival at varying relative humidities indicate that there is a mid-range of relative humidity, approximately between 40% and 70%, that minimizes the combined survival or infectivity of these organisms. The available data suggest that the actual incidence of airborne-transmitted diseases in humans should be lowest in indoor environments with mid-range relative humidities, given similar rates of occupancy and ventilation.
Epidemiological Studies on Respiratory lnfections
Several investigators have noted that the incidence of respiratory infections increases in winter when people are exposed for long periods of time to low indoor humidity levels (34,37,42). Nine epidemiological studies have provided further information on this hypothesis. Eight of these studies examined the effect of increasing relative humidity from low to mid-range levels by using humidifiers and one study examined the incidence of respiratory infections in homes with high versus
mid-range relative humidities.
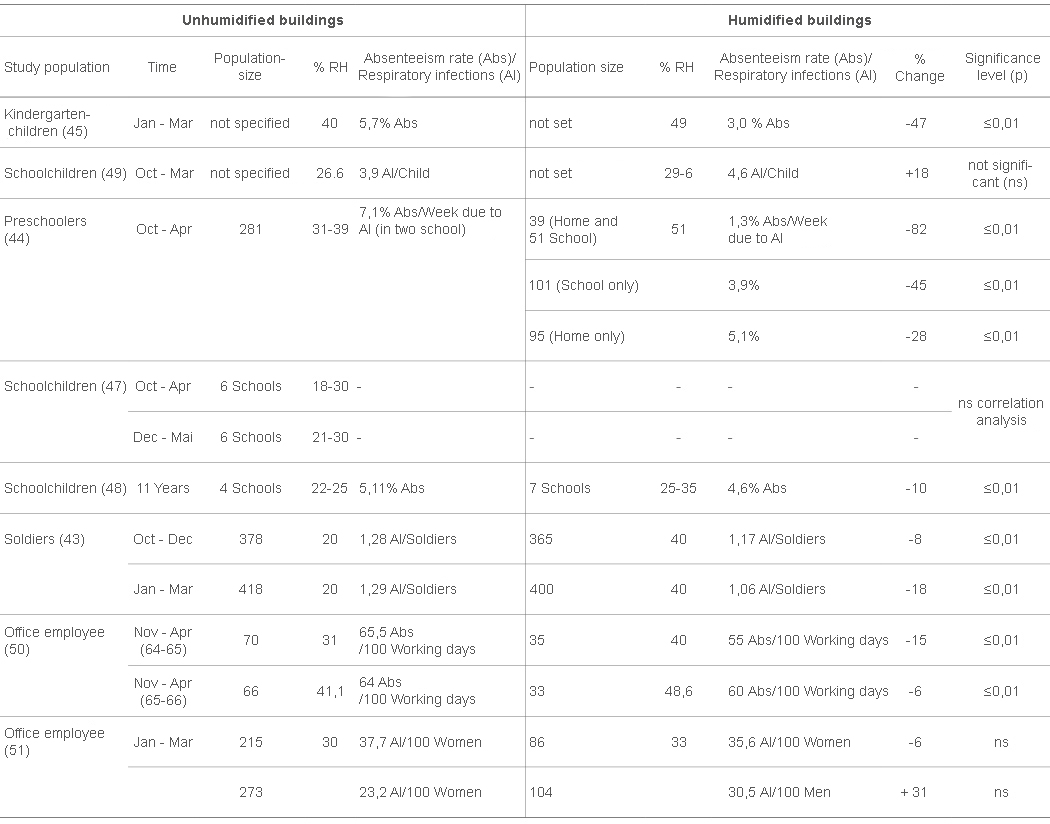
Gelperin (43) examined the relationship between indoor relative humidity and the incidence of respiratory illness among 800 army recruits in two barracks, one of which was humidified. Ventilation rates were carefully controlled. The relative humidity averaged 20% in the unhumidified barrack and 40% in the humidified barrack. There were 8% fewer upper respiratory infections among soldiers in the humidified barrack between October and December and 18% fewer infections between January and March compared to recruits in the barrack without humidification. Sale (44) found a significant reduction in respiratory infection among children attending a humidified school. The effect was intensified if the home was also humidified. The children were divided into four groups depending on the presence or absence of humidification in the school and/or home. The average weekly absentee rate due to respiratory infections was 7.1% for children without humidification at school or at home, 5.1% for children with humidification at home only, 3.9% for children with humidification at school only, and 1.3% for children with humidification at school and at home.
Ritzel (45) noted a decrease in colds, sneezing, sore throats, and fever in kindergarten children after the average relative humidity in the kindergarten was increased from 40 to 49%. Several studies have used absentee rates as an estimate of respiratory infections since approximately 50% of absenteeism from school or work is caused by viral respiratory diseases (46). Green (4 7) correlated daily winter relative humidity levels and absentee rates for six schools in Saskatoon and six in Halifax. Absentee rates decreased with an increase in relative humidity but the correlation was not statistically significant. A second study by Green (48) combined data for 11 years from 12 Saskatoon schools and found a statistically significant linear correlation between relative humidity and percent absenteeism. Absenteeism dropped by 20% as the average relative humidity increased from 22% to 35%.
Conversely, Sataloff and Menduke (49) found a higher incidence of illness in children from a humidified versus a nonhumidified school. However, the relative humidity in the humidified school was only 3% greater than in the nonhumidified school and the difference in illness rates was not statistically significant. The relationship between absentee rates and humidity was examined in two studies on Swiss office workers. Serati and Wuthrick (50) reported significantly fewer absences in a humidified versus nonhumidified office. On the other hand, Guberan et al. (51) did not find a significant difference in a similar study that examined absenteeism due to respiratory infections.
Melia et al. (52) compared the incidence of respiratory conditions such as colds, wheezing, and bronchitis among English children with several factors in the home environment. The relative humidity was measured in the children‘s bedrooms and exceeded a mean weekly value of 55% for 74% of the homes. There was a higher incidence of respiratory conditions among 31 children from homes with mean weekly humidity levels above 75% compared to 125 children from homes with lower mean relative humidity levels. The difference was statistically significant for boys. There were no significant differences in the incidence of respiratory conditions among children from homes with mean relative humidities below 55% versus the 55 to 74% range. Furthermore, no statistically significant relationships were found between the incidence of respiratory infections and the children‘s age, sex, class, home temperature, or parents‘ smoking habits.
Epidemiologische Studien zur relativen Luftfeuchtigkeit (r. F.) und zu Infektionen der Atemwege (AI)
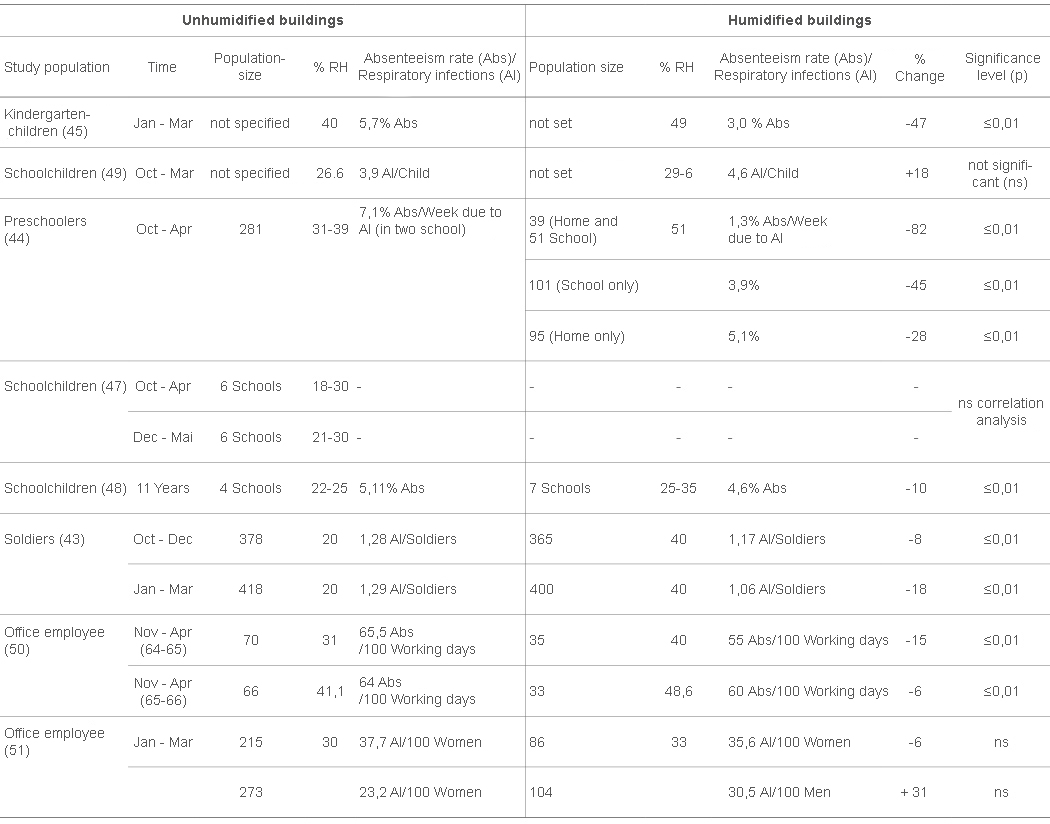
Table 1 summarizes the results of the eight epidemiological studies on the incidence of respiratory infections or absenteeism among the occupants of buildings with low versus mid-range relative humidities. Five out of the eight studies found a statistically significant reduction in respiratory infections/absenteeism among people in humidified buildings. One study found a nonsignificant reduction in absenteeism among children attending a humidified school, and two studies found an increase in absenteeism among people exposed to humidification, though the results were not statistically significant. The single study with data on high relative humidities found significantly more respiratory conditions among boys from homes with very high relative humidity levels. Therefore, the epidemiological evidence, combined with the results on bacterial and viral survival at various relative humidities, tends to support the conclusion that the incidence of respiratory infections is partially dependent upon the indoor relative humidity and is reduced by a change in relative humidity from low or high to midrange (40-60%) levels. The epidemiological evidence cannot, however, be considered as conclusive, as many of the studies did not carefully control for possible confounding variables such as ventilation and occupancy rates. Both a decrease in the fresh air ventilation rate and an increase in the occupancy rate in winter can partly account for the seasonal incidence of respiratory infections. The ventilation rate has been shown in animal experiments (39) to significantly affect the incidence of respiratory infections and the occupancy rate has been found in field studies to affect the number of infections during influenza epidemics (53,54). The specific mechanism by which mid-range relative humidities might decrease the incidence of respiratory infections cannot be determined from the available studies. The decrease might be due to alterations in aerosol settling rates, a decrease in the survival of airbornetransmitted viruses (and possibly in the survival of viruses, attached to surfaces such as dishes and furniture, that are transmitted by direct contact) or to a decrease in human susceptibility to infection. The latter possibility has been considered by Lubart ( 7,8) and Zeterberg (9), who suggested, on the basis of case reports, that low humidities increase susceptibility to common colds after direct contact has occurred by drying the protective mucous membranes of the nose and throat. As discussed earlier, there is presently little experimental or epidemiological evidence for this view. lt is possible that the dry patches noted by Lubart in the throat and nose of patients were the result of, and not a contributing cause of, infection.
Relative Humidity and Allergens
About 10% of the population is estimated to suffer from allergies (55). The abundance of two major causes of allergy, mites and fungi, increases proportionately with the average indoor relative humidity. An additional problem is introduced by humidification equipment which can generate aerosols that are contaminated with fungi or bacteria that cause allergic diseases such as asthma, rhinitis and hypersensitivity pneumonitis.
Mites
Mites are the most important cause of house dust allergies. Laboratory studies have determined that populations of the common house mite, Dermatnphagoides pt,eronyssinus, reach a maximum size during exposure to 80% RH (56).
Several field studies have found that the number of mites in residences closely parallels seasonal changes in the indoor relative humidity. In addition, mite populations were almost eliminated in winter when the relative humidity feil below 40 to 50%. For example, Korsgaard (57), in a sample of 98 houses, found fewer than 10 live mites per gram of house dust when the relative humidity was below 45%. Arlian et al. (58), in a two-year study of mites in 19 houses, found that the number of mites per gram of dust varied between 400 to 1100 at 70% RH but fell to fewer than 50 at 40% RH. Murray and Zuk (59) in a two-year study of mites in two houses found no mites at all when the indoor relative humidity feil below 50%. The studies by Korsgaard and Arlian et al. also found that the indoor relative humidity was the most important determinant of mite abundance. Both studies found that mite density was unaffected by the age of the building or by the thoroughness of house cleaning. Korsgaard also examined the relationship between relative humidity, mites and ailergies, among 75 patients with mite allergies and 23 nonallergic controls. The median relative humidity in the patients‘ houses was 50% compared to 43% among the controls. The difference boarded on statistical significance with p = 0.054. The number of mites per gram of dust was also consistently higher in the patients‘ houses compared to the controls over three sampling locations. The results suggest the possibility of a direct cause and effect relationship between higher average indoor relative humidities and allergies due to mites. Humidification can have a significant impact on mite abundance. One study found an average of 703 mites per gram of dust in six humidified houses versus 197 in nine houses without humidification (60).
Fungi
Fungi known to cause ailergic reactions such as asthma or rhinitis are of the genera Alternaria, Cladosporium, Aspergillus, Mucor, Rhizopus, and Merulius. (61). Several fungi such as Aspergillus can also cause hypersensitivity disease in individuals that do not normally suffer from allergies (62). The majority of fungi require relative humidities in excess of 75% in order to grow. Consequently, actively growing fungal populations are usually limited to areas such as kitchen and bathroom walls and window frames subject to frequent condensation as a result of locally high relative humidities (61). Ceiling tiles in office buildings can be a common source of fungal contamination, especiaily in buildings with ceiling-mounted air ducting systems, as the tiles may be directly exposed to moisture when the air conditioning system is in use. In addition, damp organic material such as leather, cotton, paper furniture stuffing, and carpets can be contaminated with fungi (1). A cause-and-effect relationship between high indoor relative humidities and ailergies is complicated by the fact that many of the allergenic fungi are ubiquitous in both the indoor and outdoor environment. Consequently, it can be difficult to determine if a fungal ailergy is the result of outdoor or indoor exposure or if indoor fungal contamination is derived from indoor or outdoor sources. However, Solomon (63) found higher average relative humidities and fungal isolates per cubic meter of indoor air between December and March in the homes of 92 patients with allergies compared to the homes of 58 controls without allergies. The relative humidity averaged 35.5% with 342 isolates per cubic meter of air in the patients‘ homes compared to an average relative humidity of 26% and 226 isolates for the control group.
Humidifiers
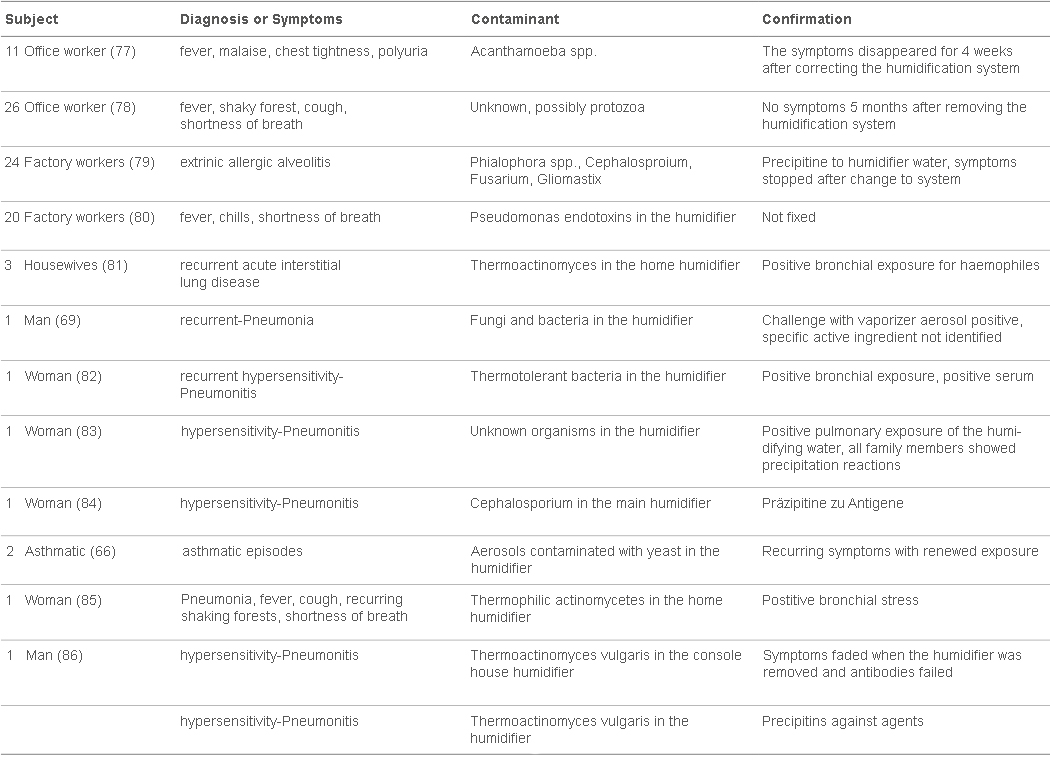
Humidifiers have both a positive and negative effect on allergies. The beneficial effect of humidification on allergies was shown by a study that examined the effect of home humidification on 817 patients with allergies; 65% of the patients reported an excellent improvement in their condition, and 30% reported a good improvement after home humidifier installation and use. The subjects reported a decrease in the dryness of the nose and throat and improved nasal and bronchial breathing during humidifier use (10). On the other band, humidification equipment is frequently contaminated with allergenic bacteria, protozoa, or fungi that can cause allergies if they are disseminated into the air. Microorganisms in humidifiers can proliferate at a very fast rate under favorable temperature and moisture conditions and be circulated as an aerosol throughout an entire building. The process of growth and continuous recirculation increases both the amount and duration of exposure and can increase the possibility of effective contact. Humidifier contamination is a particularly serious problem in hospitals where opportunistic bacteria and fungi disseminated by humidifiers have been found to cause serious infections in immunosuppressed patients (64,65). Humidifiers have been found to be contaminated with the fungi Aspergillus (66), Micropolyspora species (67), Alternaria, Penicillium, Mucor, and Aspergillus (68), and Hormodendrum, Ustilago, Rhodotorula and Crytococcus (69); the bacteria Staphyl,ococcus aureus (68), Pseudomonas aeruginosa (7 0), Enterobacter species (71), and Acinobacter species (65); and the allergenic amoebae Naegleria gruberi and Acantharrwebae (72, 73).
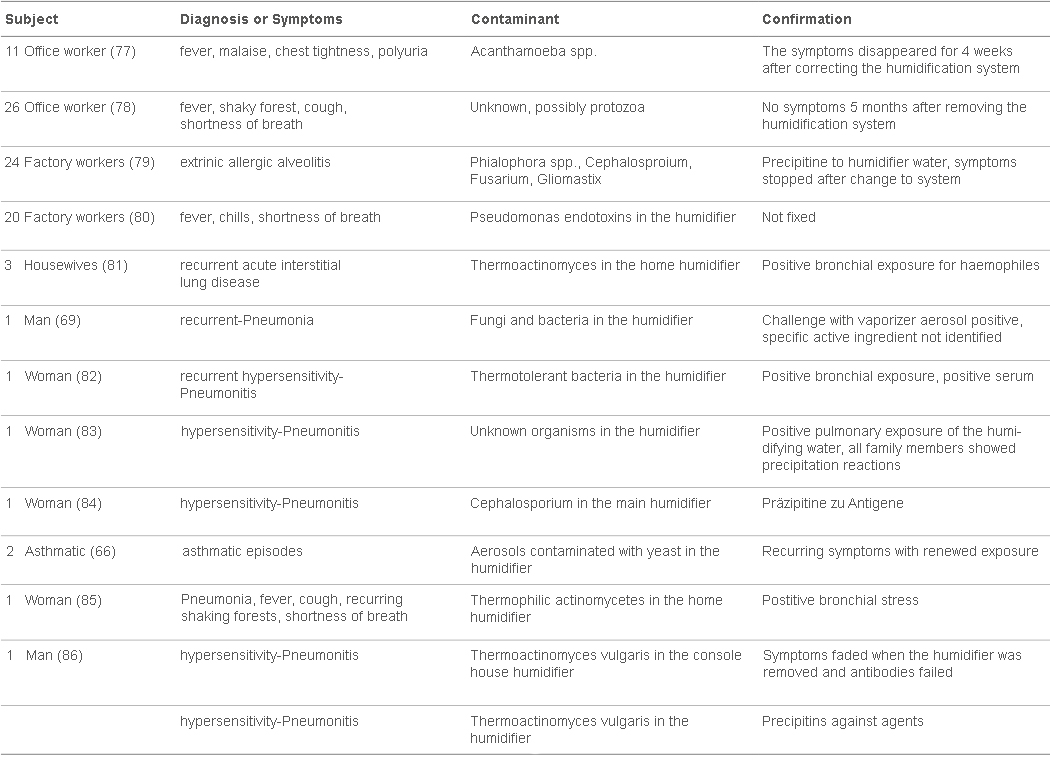
Epidemics of disE!ases caused by Legionella pneurrwphila in hospitals and offices have been traced to contaminated air conditioning equipment and cooling towers but there are no reported cases of Legionnaire‘s Disease attributable to humidifiers. Humidifi.er water temperatures are usually below the temperature range of 35 to 40°C preferred by Legionella. However, L. pneumophila was found in a hospital humidifier and was shown experimentally to cause an immunological response in guinea pigs (74). This suggests that contaminated humidifiers can potentially cause L. pneumophila infections in humans. Most humidifier-related health problems are caused by humidifiers which draw water from a reservoir and generate a cool mist. The mist can readily disperse small particles of contaminants growing in the water reservoir. Evaporative humidifiers are designed to produce only water vapor which is not contaminated with other particles. Burge et al. (75) sampled 111 mostly evaporative domestic humidifi.ers and found microbial contamination rates of 77 to 89%. In this case, the humidifi.ers did not appear to cause contamination of the indoor air. In another study, however, evaporative humidifiers were linked to an increase in the number of bacteria in the air of hospital rooms suggesting that some evaporative humidifiers can produce a small amount of aerosol in addition to vapor (71). Evaporative humidifiers can also produce contaminated aerosols if the humidifi.er fan blows air through a contaminated filter (76). There are a large number of reported cases of allergic diseases that have been traced to humidification equipment. Table 2 summarizes the results of several reports on allergies and hypersensitivity disease caused by the use of humidifiers in residential, office, and factory environments (66,69,77-87).
Relative Humidity and Noxious Chemicals
Several chemicals that can be found in indoor air interact with water vapor to form respiratory and dermal irritants. Health problems attributable to chemical interactions with humidity are probably less widespread than problems caused by biological interactions. However, chemical interactions can be important in buildings with a high proportion of formaldehyde-containing materials, gas stoves for cooking, or geographically located near outdoor sources of water-reactive air pollutants.
Formaldehyde
Low-level exposure to formaldehyde has produced adverse health effects such as irritation to the skin, eyes and throat, respiratory disorders and allergies (1).
As formaldehyde is water-soluble, high relative humidities promote the off-gassing of formaldehyde from ureaformaldehyde foam insulation and from numerous other sources such as plywood, paper and other wood products, carpets and textiles (88). A climate chamber investigation into the rate of off-gassing of formaldehyde from chipboard found that formaldehyde concentrations in the air were directly proportional to the relative humidity at a given temperature. Formaldehyde levels increased from 0.5-0.6 rng/rn3 at 30% RH to 1.2-2.0 rng/rn3 at 70% RH (89). A field study of forrnaldehyde levels in 20 hornes found a statistically significant (p < 0.01) coITelation between the indoor relative hurnidity and the forrnaldehyde concentration in the air (90).
Sulfur and Nitrogen Dioxides
Sulfur dioxide acts as a respiratory irritant in healthy subjects and causes bronchial constriction in sensitive individuals such as asthrnatics at concentrations as low as 0.1 pprn (91). Sulfur dioxide cornbines with water vapor to form aerosols containing sulfate salts and sulfuric acid which are rnore irritating than sulfur dioxide itself (92). Nitrous and nitric acids are forrned indoors by the interaction of water vapor with nitrogen dioxide frorn unvented gas cooking stoves and heaters. Both acids are thought to play an etiological role in the developrnent of respiratory illness and decreased pulrnonary function (93).
Ozone
Indoor ozone levels are enhanced by low relative hurnidities whereas high relative hurnidities reduce ozone concentrations by accelerating the adsorption of ozone rnolecules onto indoor surfaces (94). Ozone is a strong oxidizing agent and in the exposure range likely encountered in a residence, acts as an irritant to the eye and rnucous rnernbranes (95).
Occupational Dermatoses
The nurnber of cornplaints of skin irritation such as urticaria, erytherna, and eczerna arnong ernployees of several factories and a telephone exchange building decreased after the relative hurnidity was increased frorn 30 to 40% to above 50%. Skin irritation rnay have been partly caused by an interaction between low relative hurnidities and chernicals such as trichloroethylene (96), cyanoacrylate (97), and a rnethacrylate polymer (98).
Conclusions
This review of the indirect health effects of relative hurnidity indicates that adverse health effects would be rninirnized by rnaintaining relative hurnidity between 40 and 60%. Presently indoor relative hurnidity levels below 40% are widespread in winter. An increase in low relative hurnidities to above 40% should reduce the incidence of respiratory infections, the severity of allergic and asthrnatic reactions, and indoor ozone levels. Relative hurnidity levels above 60% can occur in surnrner, especially in air-conditioned buildings, or in kitchens and bathroorns during the winter. A reduction in high relative hurnidity levels to below 60% should reduce the abundance of allergenic rnites and fungi and the concentration of forrnaldehyde, and acids and salts of sulfur and nitrogen dioxides in the air.
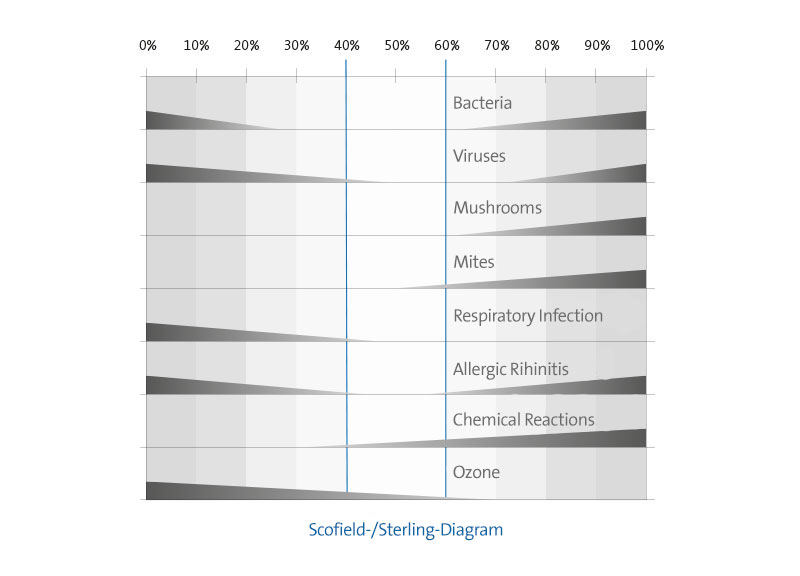
The effect of relative hurnidity on biological and chernical factors is graphically surnrnarized in Figure 1. The shape and height of the bars in the figure are only suggestive of an increase or a decrease in effect and do not represent quantitative data. Most of the health effects either increase in severity above 60% and/or below 40% relative humidity. The exceptions are most chemical interactions which consistently increase above 30% and conditions that produce ozone, which consistently increase in severity with a decline in relative humidity. The shaded portion of the graph indicates the approximate optimum mid-range zone für minimizing adverse health effects attributable to relative humidity. The adverse health and comfort effects of low relative humidities indicate that the use of humidifiers should be encouraged in regions with low indoor relative humidities during winter. A decrease in morbidity and possibly mortality due to influenza may be the most important beneficial result of an increase in relative humidity from low to mid-range levels.
However, humidification equipment must be properly maintained and sterilized in order to prevent microbial contamination. Unfortunately, commonly used humidifier sterilants such as bleach have not been effective in preventing humidifier contamination (75). Sterilants can also introduce a new set of health problems if the sterilant itself is disseminated by the humidifier. For this reason it may be preferable to encourage the use of evaporative versus aerosol-forming humidification systems as there are fewer dissemination problems associated with the former system. Another option is to use steam as a humidifying aerosol.
Humidification must also be approached cautiously, as an increase in the average relative humidity may cause structural damage to the building or result in pockets of high relative humidity leading to undesirable mite or fungal growth. Structural damage is most likely in older buildings without vapor barriers as moisture can diffuse into the wall and condense on the outside sheathing. For example, condensation on the sheathing surface of an uninsulated house without a vapor barrier will occur when the outdoor temperature falls below -10°C and the indoor relative humidity exceeds 15% (99). Pockets of high relative humidity occur in most buildings because of variations in the location of humidity sources and room ventilation rates. This problem indicates that average relative humidities throughout a building should be kept, if possible, at the low end ofthe suggested range ofrelative humidity. The indirect health effects ofrelative humidity may be growing in importance as a result of the continuing construction of energy efficient sealed buildings with low fresh air ventilation rates. The high fresh air ventilation rates found in older leaky buildings may dilute the concentration of pathogens, allergens and noxious chemicals in the indoor air and thus offset some of the health problems associated with relative humidity. In contrast, energy-conserving buildings require the careful maintenance of good indoor air quality through maintaining, among other factors, optimum relative humidity levels in order to minimize potential health problems.