Study from Ali A. Abusharha, BSc
Dry eye can be caused by either internal (milieu interieur) or external (milieu exterieur) factors.1 The external factors include humidity, temperature, air velocity, and air pollution.
2 As an exposed structure, the precorneal tear film is exposed to different environmental conditions that may affect its parameters dramatically. Studies investigating the effect of relative humidity (RH) on tear film using an air pump to direct dry air into an eye goggle found that the mean tear film evaporation rate is doubled as a result of a decrease in RH of 20% in patients with dry eyes and meibomian gland dysfunction.
3
Other studies using the same technique have shown that the average increase in evaporation rate of tear film among normal and dry eye patients was between 28% and 59% when the RH decreased by 10%.
4 Recently, a crossover study of patients with dry eyes using artificial tear solution has shown that the tear evaporation rate was increased by 35% as the RH decreased from 35% to 45% to 25% to 35%.5.
In addition to an alteration in tear film evaporation rate, other parameters such as tear production and break-up time have been found to be affected by adverse environments. Noninvasive tear break-up time (NIBUT) was investigated in mild dry eye patients wearing contact lenses in different environmental conditions. The mean NIBUT value decreased from 12.42 to 8.3 seconds (without contact lens) and from
5.34 to 4.90 seconds (with contact lens) as the RH decreased from 34% to 19%.
6
An animal model study (BALB/c mice) has shown that exposure to a dry environment could result in a significant decrease in tear production, increase in fluorescein staining, and decrease in goblet cell density.7 Korb et al8 demonstrated that tear lipid layer thickness (LLT) increased significantly in dry eye patient when the humidity increased. Unfortunately, most of these environmental factors cannot be avoided. Ocular symptoms including itching, burning, and irritated eye are commonly reported by individuals working in closed and dry environmental conditions, such as offices or aircraft cabins, which are characterized by low humidity.
9–12
The purpose of this study was to determine whether any effects on preocular tear film are produced by exposure to a low RH adverse environment. It also probes the relationships between tear film parameters to understand the mechanism of the signs and symptoms of dry eyes that may be induced by a desiccating environment.
Methods
The effect of RH on the tear film was assessed in this study. All procedures were approved by the human ethics committee of the Glasgow Caledonian University. Two visits were required to carry out this study. One visit was to assess the physiological tear film parameters in normal humidity. The other visit was to expose the tear film to a very dry environment and then assess the tear film parameters. The visits were arranged in an alternating manner.
Twelve healthy normal subjects (10 men, 2 women) with no symptoms of dry eye were enrolled in this study (mean age 29.8 ± 3.3 years) (Ocular Surface Disease Index13 score < 10 points and NIBUT > 10 seconds).
Study Design
To monitor the changes in tear film behavior during exposure to a dry environment, tear film parameters were observed at 20-minute intervals for 1 hour starting from the baseline assessment at 0 minute (0, 20, 40, and 60 minutes) while at normal RH only one observation was made after 15-minute equilibration (Fig. 1).
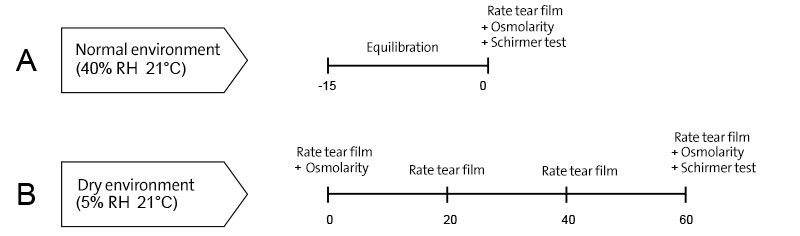
FIGURE 1. Study design. A, In normal environment (40% RH/ 21°C), tear parameters include evaporation rate, ocular surface temperature, lipid pattern, tear breakup time, ocular comfort, osmolarity and Schirmer test were assessed after 15 min of room adaptation. B, In a low humidity condition (5% RH/ 21°C) tear film physiological investigations were carried out immediately (0 min) then at 20, 40 and 60 min time points. Tear parameters described above were assessed at all time points except tear osmolarity and production. Tear osmolarity were measured only at 0 and 60 min time points while Schirmer test was performed at 60 min time point only.
To create an adverse controlled environmental condition, a controlled environment chamber (CEC; Weiss-Gallenkamp Ltd, Loughborough, United Kingdom) was used. The CEC is 2.2 x 2.3 x 2.3 m in size and is able to produce a temperature between 5°C and 35°C and an RH of 5% to 95%. The temper- ature variation and fluctuation in the CEC are ±2°C and ±1°C, respectively, whereas the RH fluctuation is ± 3%. To study the effect of RH on tear film, the CEC was set at 2 conditions. These conditions were as follows:
- Normal environment: ambient temperature at 21°C and 40% RH
- Dry environment: ambient temperature at 21°C and 5% RH
Such an adverse environment has been reported to be experienced by airline crew and high-technology device manufacturers where the minimum recorded RH can be less than 5%.9,14 The Workplace Health Committee has reported that the minimum recommended RH in indoor workplaces is 40%, whereas the ambient temperature should be between 19°C and 22°C.
15
In brief, the tear film parameters measured were tear evaporation rate, osmolarity, LLT, tear production, stability, ocular surface temperature (OST), and ocular comfort. These parameters were assessed for each subject in both normal and dry conditions.
The tear evaporation rate was measured using a Servo-Med Evaporimeter (Servo Med, Varberg, Sweden)
16, whereas stability and the tear lipid layer were evaluated by Keeler TearScope-Plus (Keeler Ltd, Windsor, United Kingdom).17
The thickness of the lipid layer was assessed by TearScope and graded using the system described by Guillon.
17The OcuSense Tear Lab osmometer18 was used to measure tear osmolarity at 3 time points for one eye only because of the high cost of the disposable test chips. Because of its invasive nature, Schirmer strips19 (Clement Clarke International Ltd, Harlow, Essex, United Kingdom) were used to measure tear production only at the end of the experiment. A modified questionnaire was used to assess the ocular comfort.
20 The subjects were asked to indicate their responses by marking a vertical line on a visual analogue scale21
21 instead of reporting the category of response.
To monitor the changes in OST during exposure to a dry environment, a FLIR Systems ThermaCAM P620 (FLIR Systems, Surrey, United Kingdom) was used. The camera is self calibrating and comes with high-definition detector (focal plane array, 640 x 480 pixels) that is thermally sensitive to ±0.06°C and detects a temperature range between -40°C and +500°C. A close up lens with spatial resolution of 50 µm was attached to the camera to provide a clear and focused image of the ocular surface.
The data obtained by the camera were transferred to computer via Firewire cable and then analyzed using ThemaCAM Researcher Professional version 2.9 software (FLIR Systems). All data were statically analyzed using PASW Statistics version 18 (IBM corporation, Somers, NY). A test of normality was carried out first using a Kolmogorov–Smirnov test. Normally distributed data were compared using a repeated measured analysis of variance and Tukey post hoc test. Data not normally distributed were compared using Friedman test and a post hoc Wilcoxon rank sum test. Correlation between parameters was derived using a Pearson correlation for normal distributed data. Data not following a normal distribution was correlated using a Spearman rho test.
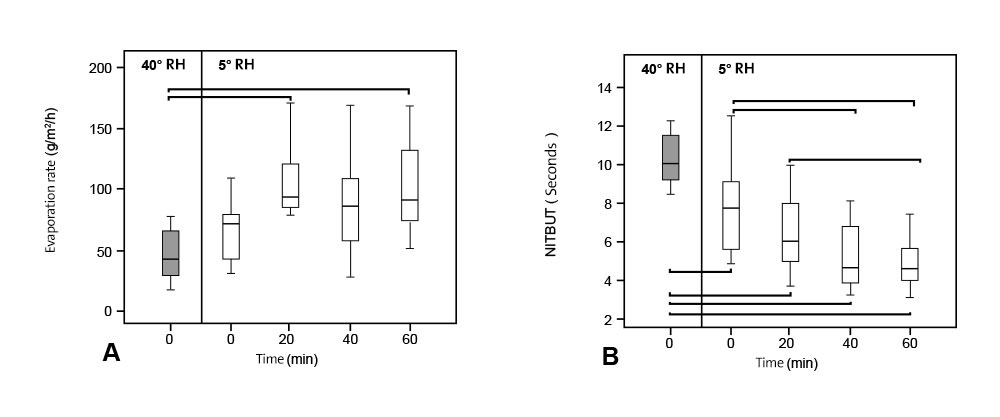
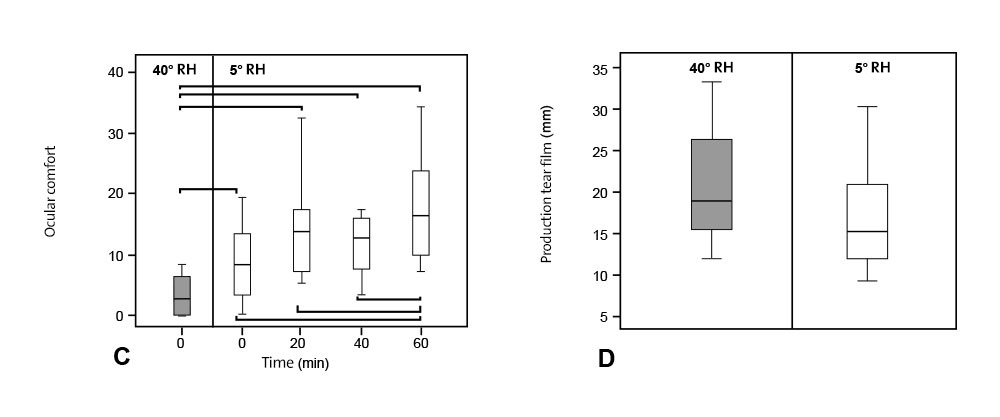
FIGURE 2. A box plot showing tear evaporation rate (A) measured at normal humidity (40%), immediately after exposure to dry environment (0 min) then at 20, 40 and 60 min time points. Significant increase in tear evaporation was found during exposure to adverse environment. NITBUT (B) became shorter when tear film was exposed to dry environment. Significant difference was seen in ocular comfort (C) and reduction of tear production (D).The box represents the interquartile range that contains 50% of the values. The whiskers are lines that extend from the box to the highest and lowest values, excluding outliers (O) that are 1.5 to 3 box lengths from the upper and lower edge of the box and extremes (*) that are more than 3 box lengths. The line across the box indicates the median value. Pairwise significant differences are shown (*).
Parametric testing showed no significant difference between evaporation rate at baseline measurement, at 40% and 5% RH. Tear evaporation rate at 40% RH and 5% RH is shown in Figure 2A. But a significant difference was found between 40% and 5% RH at 20-minute (P = 0.007) and 60-minute (P = 0.004) time points. The mean tear evaporation rate doubled from 0.13 mL/minute (46.08 g/m2/h) in the normal environment to 0.28 mL/minute (101.43 g/m2/h) after exposure to low humidity for 60 minutes. To put this change in context, it has been reported that the cut-off value of the evaporation rate between normal and dry eye patients is between 0.20 and 0.22 µL/minute.
22
A box-plot of NIBUT is shown in Figure 2B. Unlike the evaporation rate, there was a significant difference even on immediate exposure (0 minute; P = 0.008). NITBUT at all time points (0, 20, 40, and 60 minutes) at 5% RH were significantly lower than the values observed at 40%. In the dry environment, no significant difference was found between 40 and 60 minutes where the median values were 4.82 and 4.75 seconds, respectively, and a plateau in NITBUT was observed. It should be remembered the consensus that when tear break-up time is less than 5 seconds, then this value is considered as severe dry eye syndrome (DEWS grade 3 dry eye).
1
LLT was significantly lower at all time points (0, 20, 40, and 60 minutes) in the dry condition compared with the humid environment. Furthermore, LLT continued to decrease significantly until 40-minute exposure. No significant difference was observed between 40 and 60 minutes, suggesting a plateau had been reached. Data are not shown due to the limited number of grades observed.
Although tear osmolarity increased from 292 mOsm/L at normal humidity to 298 mOsm/L on immediate exposure to a dry environment, there was no statistically significant difference in tear osmolarity between that observed in the normal and in the desiccating environment (P = 0.09).
Ocular discomfort was significantly higher at 5% RH (P = 0.02). It should be noted that dryness and itchiness were the most commonly reported symptoms in the dry environment. Significant changes between normal condition and desiccating condition are shown in Figure 2C with an asterisk.
A significant decrease in tear production was found between 40% and 5% RH (P = 0.02) (mean wetting length 20.33 and 16.50 mm, respectively). Figure 2D shows the changes in tear production at normal and dry conditions.
Previous studies have suggested that ambient environmental conditions could affect tear film behaviour.9,23 The aim of this study was to determine the relationship between the tear film and RH and also to observe tear film response over a period of 60-minute exposure to a dry environment. In this study, investigations of tear film parameters were carried out to understand the mechanism of the changes that occur in the tear film at these low humidity adverse environments.
It is clear from this study that the lipid layer is significantly thinner after exposure to a dry environment. Recently, many proteins have been reported to be present in the tear lipid layer.
24,25 These proteins are known to interact with meibomian lipids, forming a thin polar phase that plays an important role in maintaining a stable spread of lipids over the aqueous phase.26 Other works have shown that a change in RH can cause protein structural reorganization because of alteration in protein oxidation rate and denaturation.
27–29 These changes in protein properties could explain the thinner tear film lipid observed at low humidity.
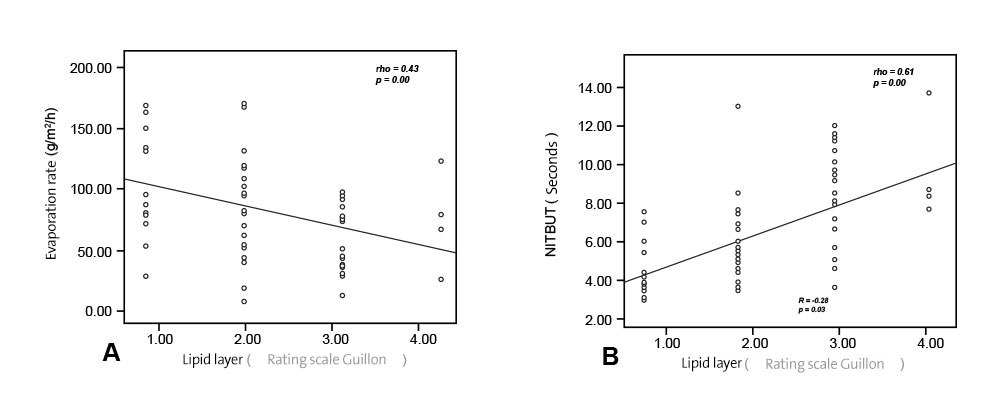
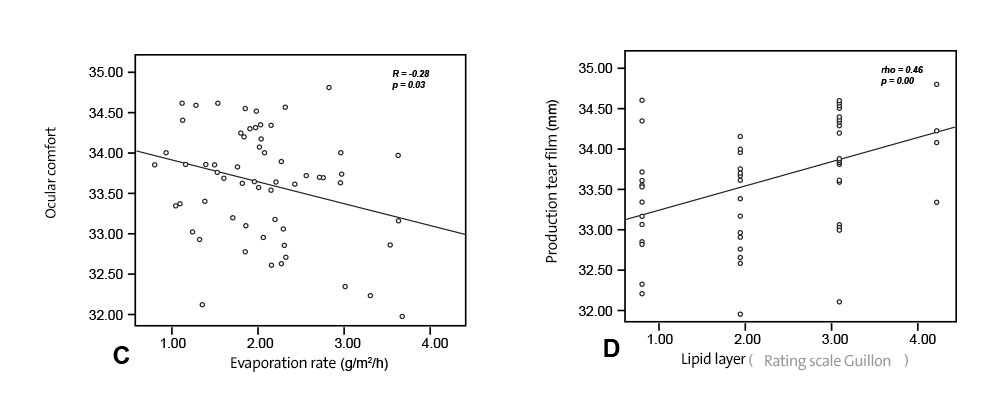
FIGURE 3. Scatter plot showing correlation between evaporation rate and lipid layer thickness (A), tear break up time and lipid layer thickness (B), ocular surface temperature and lipid layer thickness (C).
The evaporation rate of the tear film increased sharply during exposure to the dry environment and tear stability was significantly lower. Both these findings agree with previous reports.
3 This is also consistent with reports that an elevated evaporation rate is associated with thin and abnormal lipid patterns.
30 This reflects the fact that one of the main functions of the tear lipid layer is to prevent excessive evaporation of the aqueous layer.
31 In this study, significant correlations were found between evaporation rate and LLT (rho = -0.43, P = 0.00; Fig. 3A), evaporation rate and NIBUT (rho = -0.47, P = 0.00), and NIBUT and LLT (rho = 0.61, P = 0.00; Fig. 3B). This confirms the intimate interrelationship between these parameters.
30
Adequate production and clearance of tears is essential to maintain a stable tear film and a healthy ocular surface.
32Therefore, any reduction of tear production could cause aqueous deficient dry eyes
33 and lead to signs and symptoms of dry eyes.34 Aqueous deficient dry eye is considered as one of the major classes of dry eyes.
1 A previous animal model study has found that tear secretion is decreased after exposure to a low RH environment.
7 Likewise, in this study we found that tear production decreased significantly.
The reduction of aqueous secretion during exposure to the dry environment could be because of a decrease in response to irritation caused by Schirmer insertion. In the current study, a short NITBUT and poor tear film stability were observed under dry environ- mental conditions. Therefore, the ocular surface afferent sensory nerves may have been habituated to constant stimulation as a result of ocular surface desiccation and are thus not reacting to stimulation caused by the Schirmer strip.
35
During exposure to the desiccating environment, it could be expected that tear production would increase to compensate for increased evaporation and tear osmolarity. This compensatory mechanism would act to maintain the homeostatic integrity of the ocular surface environment. This was not observed. However, this could be because of tear production only being measured at 60-minute postexposure. Intervening observations may have shown an initial increase in production, which had already abated by the time of the observation.
An increase in tear osmolarity after exposure to the low humidity environment was seen, but this elevation did not reach significance (P = 0.09). The mean tear osmolarity changed from 292.8 at normal humidity to 298.5 and then to 296.9 mOsm/L after exposure to the desiccating environment for 0 minute and 60 minutes, respectively. As a reduction in tear production and an elevation in tear evaporation rate were observed in this study, one would have expected to see an increase in osmolarity.
36
This was not the case and could be a result of the limited size of the study. A power equation found that a sample size of 50 subjects would be required to confirm a significant difference in osmolarity.
It is clear from these data that in healthy normal subjects exposed to adverse environmental conditions, homeostatic compensatory mechanisms play a role in maintaining important tear film parameters. In theses healthy normal subjects, osmolarity was unchanged but other parameters, such as NITBUT, evaporation rate, LLT, tear production, and ocular comfort, all showed significant changes. In dry eye subjects, it is likely that the homeostatic response would not be as robust and the ocular surface functional unit would not be as responsive to environmental change.
35 This is likely to lead to a more pronounced perturbation and greater symptoms in this group when they are exposed to adverse environments.
Recently, a number of studies have reported complaints related to time spent in indoor or artificially ventilated environments such as offices or aircraft cabins.
9,10 Symptoms such as itching, burning, or irritated eyes are commonly reported among office employees and airline crew members.
11,37 In this study, ocular discomfort was found to be significantly higher in a dry environment. This finding in subjective discomfort reflects the objective findings of increased evaporation rate, increased instability of tear film, and reduction in tear production. In this study, dryness and itchiness symptoms were the most commonly reported by subjects compared with other dry eye symptoms in the questionnaire (gritty, stingy, tired, and painful).
Infrared thermography is an efficient noncontact tool to measure OST.
38 OST was measured in this study to find out if there is any effect of RH on OST. Several other studies have shown that OST can be altered by both internal and external factors.
39,40 In this study, no significant difference in mean central OST was found. However, the mean OST of the central cornea dropped by 0.61°C and 0.44°C after exposure to the dry environment for 20 and 60 minutes, respectively. To put this in context, it has been reported that the mean central corneal temperature is lower in dry eye patients by 0.20°C to 0.50°C.
41,42
Significant correlations between central corneal temperature and tear lipid thickness and evaporation rate were observed in this study (rho = 0.46, P < 0.05 and R = 0.0-0.28, P < 0.05). These correlations indicate that the dry environment does alter OST through changes to evaporation and LLT, but the magnitude of these changes are not sufficient to reach statistical significance given our sample size. However, this reduction in OST is likely to be caused by the increased cooling effect that results from elevation in tear evaporation rate. A previous study that measured OST using a contact method suggested that a decrease in RH of 6% resulted in a cooling effect equivalent to a 1°C decrease in ambient temperature.
43 However, this excessive cooling effect could be caused by other factors such as direct contact between a thermistor probe and the ocular surface or the installation of topical anaesthetic.
44
Conclusions
The present study demonstrates that the tear film is influenced by ambient environmental conditions. It is evident that there is a significant change in tear film parameters when it is exposed to a dry environment. Tear LLT, evaporation rate, ocular comfort, tear stability, and production were adversely affected by low RH. Some tear film parameters (evaporation rate, NITBUT, LLT, and ocular comfort) went from normal values to those typical of dry eyes after exposure to a low humidity environment for 1 hour. Therefore, these conditions may lead to ocular surface disorders and could also affect visual performance such as contrast sensitivity and visual acuity.
45
The effect of low RH on the anterior of the eye should be taken into consideration by people who spend long periods in dry artificially ventilated buildings and in particular airplane cabins. The environmental conditions of these locations need to be improved. If the environment cannot be improved, the tear film and ocular surface should be protected against adverse environmental conditions, particularly for those who have habitual exposure.

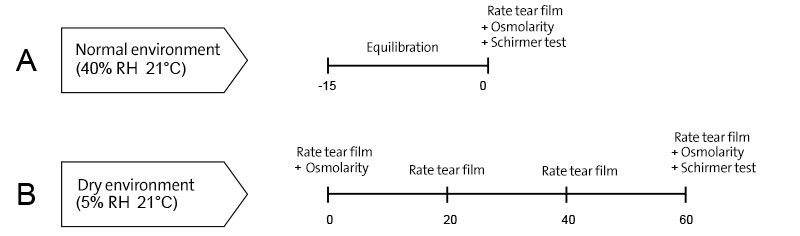
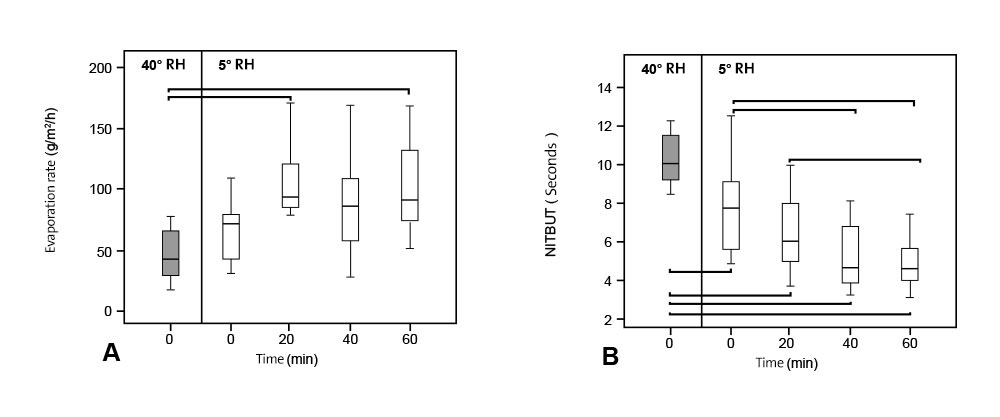
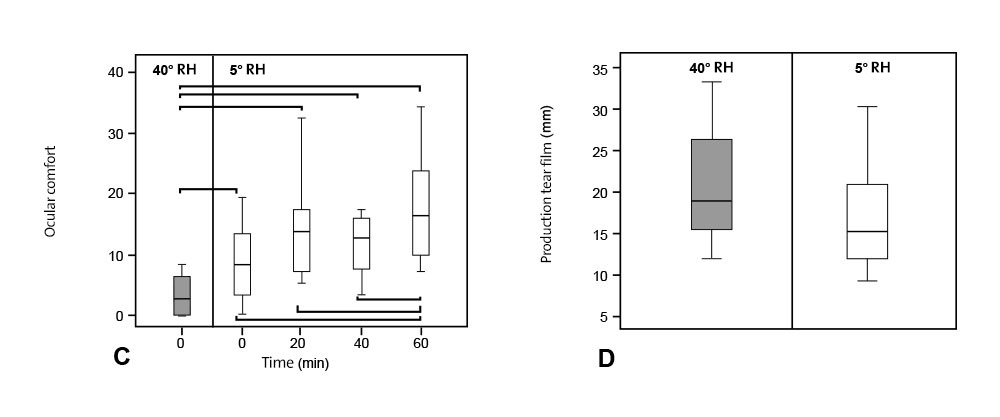 FIGURE 2. A box plot showing tear evaporation rate (A) measured at normal humidity (40%), immediately after exposure to dry environment (0 min) then at 20, 40 and 60 min time points. Significant increase in tear evaporation was found during exposure to adverse environment. NITBUT (B) became shorter when tear film was exposed to dry environment. Significant difference was seen in ocular comfort (C) and reduction of tear production (D).The box represents the interquartile range that contains 50% of the values. The whiskers are lines that extend from the box to the highest and lowest values, excluding outliers (O) that are 1.5 to 3 box lengths from the upper and lower edge of the box and extremes (*) that are more than 3 box lengths. The line across the box indicates the median value. Pairwise significant differences are shown (*).
FIGURE 2. A box plot showing tear evaporation rate (A) measured at normal humidity (40%), immediately after exposure to dry environment (0 min) then at 20, 40 and 60 min time points. Significant increase in tear evaporation was found during exposure to adverse environment. NITBUT (B) became shorter when tear film was exposed to dry environment. Significant difference was seen in ocular comfort (C) and reduction of tear production (D).The box represents the interquartile range that contains 50% of the values. The whiskers are lines that extend from the box to the highest and lowest values, excluding outliers (O) that are 1.5 to 3 box lengths from the upper and lower edge of the box and extremes (*) that are more than 3 box lengths. The line across the box indicates the median value. Pairwise significant differences are shown (*).
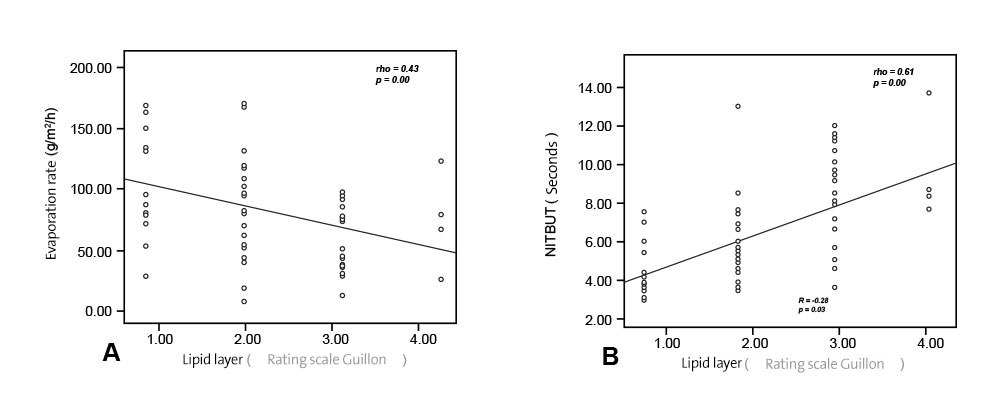
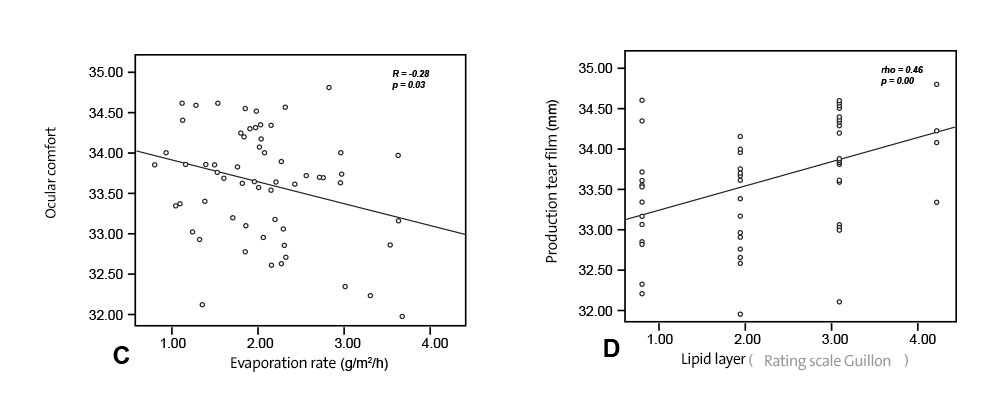 FIGURE 3. Scatter plot showing correlation between evaporation rate and lipid layer thickness (A), tear break up time and lipid layer thickness (B), ocular surface temperature and lipid layer thickness (C).
FIGURE 3. Scatter plot showing correlation between evaporation rate and lipid layer thickness (A), tear break up time and lipid layer thickness (B), ocular surface temperature and lipid layer thickness (C).