Original title: High humidity leads to loss of infectious influenza virus from simulated coughs
Source link: http://dx.plos.org/10.1371/journal.pone.0057485
Released: 27. February 2013
1. Shaman J, Pitzer VE, Viboud C, Grenfell BT, Lipsitch M (2010) Absolute
humidity and the seasonal onset of influenza in the continental United States.
PLoS Biol 8(2): e1000316.
2. Shaman J, Goldstein E, Lipsitch M (2011) Absolute humidity and pandemic
versus epidemic influenza. Am J Epidemiol 173: 127–135.
3. Hemmes JH, Winkler KC, Kool SM (1960) Virus survival as a seasonal factor in
influenza and poliomyelitis. Nature 188: 430–431.
4. Hood AM (1963) Infectivity of influenza virus aerosols. J Hyg, Camb 61: 331–
335.
5. Harper GJ (1961) Airborne micro-organisms: survival tests with four viruses.
J Hyg, Camb 59: 479–486.
6. Shechmeister IL (1950) Studies on the experimental epidemiology of respiratory
infections. III. Certain aspects of the behavior of type A influenza virus as an
airborne cloud. J Inf Dis 87: 128–132.
7. Schaffer FL, Soergel ME, Straube DC (1976) Survival of airborne influenza
virus: effects of propagating host, relative humidity, and composition of spray
fluids, Arch Virol 51: 263–273.
8. Lowen AC, Mubareka S, Steel J, Palese P (2007) Influenza virus transmission is
dependent on relative humidity and temperature. PLoS Pathog 3(10): 1470–
1476.
9. Fabian P, McDevitt J, DeHaan W (2008) Influenza virus in human exhaled
breath: An observational study. PLoS ONE 3: e2691.
10. Huynh KN, Oliver BG, Stelzer S, Rawlinson WD, Tovey ER (2008) A new
method for sampling and detection of exhaled respiratory virus aerosols. Clin
Infect Dis 46: 93–95.
11. Stelzer-Braid S, Oliver BG, Blazey AJ, Argent E, Newsome TP, et al. (2009)
Exhalation of respiratory viruses by breathing, coughing, and talking. J Med
Virol 81: 1674–1679.
12. Blachere FM, Lindsley WG, Pearce TA, Anderson SE, Fisher M, et al. (2009)
Measurement of airborne influenza in a hospital emergency department. Clin
Infect Dis 48: 438–440.
13. Lindsley WG, Blachere FM, Davis KA, Pearce TA, Fisher MA, et al. (2010)
Distribution of airborne influenza virus and respiratory syncytial virus in an
urgent care medical clinic. Clin Infect Dis 50: 693–698.
14. Hanley BP, Borup B (2010) Aerosol influenza transmission risk contours: A study
of humid tropics versus winter temperate zone. Virol J 7: 98.
15. Bjorn E, Nielsen PV (2002) Dispersal of exhaled air and personal exposure in
displacement ventilated rooms. Indoor Air 12: 147–164.
16. Qian H, Li Y, Nielsen PV, Hyldgaard CE, Wong TW, et al. (2006) Dispersion of
exhaled droplet nuclei in a two-bed hospital ward with three different ventilation
systems. Indoor Air 16: 111–128.
17. Qian H, Li Y (2010) Removal of exhaled particles by ventilation and deposition
in a multibed airborne infection isolation room. Indoor Air 20: 284–297.
18. Pantelic J, Sze-To GN, Tham KW, Chao CYH, Khoo YCM (2009)
Personalized ventilation as a control measure for airborne transmissible disease
spread. J R Soc Interface 6: S715–S726.
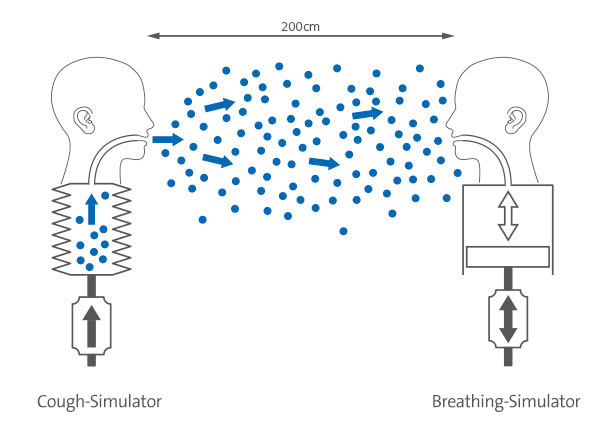
19. Noti JD, Lindsley WG, Blachere FM, Cao G, Kashon ML, et al. (2012)
Detection of infectious influenza virus in cough aerosols generated in a simulated
patient examination room. Clin Infect Dis 54: 1569–1577.
20. Lindsley WG, King WP, Thewlis RE, Reynolds JS, Panday K, et al. (2012)
Dispersion and exposure to a cough-generated Aerosol in a Simulated Medical
Examination Room. J Occup Environ Hyg 9: 681–690.
21. Blachere FM, Cao G, Lindsley WG, Noti JD, Beezhold DH (2011) Enhanced
detection of viable airborne influenza virus. J Virol Methods 176: 120–124.
22. Lindsley WG, Schmechel D, Chen BT (2006) A two-stage cyclone using
microcentrifuge tubes for personal bioaerosol sampling. J Environ Monit 8:
1136–1142.
23. ISO (2007) Respiratory protective devices – Human factors – Part 1: Metabolic
rates and respiratory flow rates. Geneva: ISO/TS 16976–1.
24. Tellier R (2010) Aerosol transmission of influenza A virus: a review of new
studies. J R Soc Interface 6: S783–S790.
25. Weber TP, Stilianakis NI (2008) Inactivation of influenza A viruses in the
environment and modes of transmission: a critical review. J Infect 57: 361–373.
26. Wein LM, Atkinson MP (2009) Assessing Infection Control Measures for
Pandemic Influenza. Risk Anal 29: 949–962.
27. Brankston G, Gitterman L, Hirji Z, Lemieux C, Gardam M (2007) Transmission
of influenza A in human beings. Lancet Infect Dis 7: 257–265.
28. Milton DK, Fabian P, Angel M, Perez DR, McDevitt JJ (2010) Influenza virus
aerosols in human exhaled breath: particle size, culturability, and effect of
surgical masks, April 18–20, Atlanta, Georgia USA. Emory Conference Center.
29. Lindsley WG, Blachere FM, Thewlis RE, Vishnu A, Davis KA, et al. (2010)
Measurements of airborne influenza virus in aerosol particles from human
coughs. PloS One 5(11): e15100.
30. Yang W, Marr LC (2011) Dynamics of airborne influenza A viruses indoors and
dependence on humidity. PloS One 6(6): e21481.
31. Teunis FM, Brienen N, Kretzschmar EE (2010) High infectivity and
pathogenicity of influenza A virus via aerosol and droplet transmission.
Epidemics 2: 215–222.
32. Brown JD, Goekjian G, Poulson R, Valeika S, Stalknecht DE (2009) Avian
influenza virus in water: Infectivity is dependent on pH, salinity and
temperature. Vet Microbiol 136: 20–26.
33. ISO (2005) Ergonomics of the thermal environment-Analytical determination
and interpretation of thermal comfort using calculation of the PMV and PPD
indices and local thermal comfort criteria. ISO 7730.
34. ASHRAE Standard (2010) Thermal environmental conditions for human
occupancy. ANSI/ASHRAE, Standard 55–2010.